

Postpartum depression: Causes, symptoms, risk factors, and treatment options
- Women and Girls

What is postpartum depression and anxiety?
It’s common for women to experience the “baby blues”—feeling stressed, sad, anxious, lonely, tired or weepy—following their baby’s birth. But some women, up to 1 in 7, experience a much more serious mood disorder—postpartum depression (PPD). (Postpartum psychosis, a condition that may involve psychotic symptoms like delusions or hallucinations, is a different disorder and is very rare.) Unlike the baby blues, PPD doesn’t go away on its own. It can appear days or even months after delivering a baby; it can last for many weeks or months if left untreated. PPD can make it hard for you to get through the day, and it can affect your ability to take care of your baby, or yourself. PPD can affect any woman—those with easy pregnancies or problem pregnancies, first-time mothers and mothers with one or more children, women who are married and women who are not, and regardless of income, age, race or ethnicity, culture, or education.
What are the symptoms of PPD?
The warning signs are different for everyone but may include:
A loss of pleasure or interest in things you used to enjoy, including sex
Eating much more, or much less, than you usually do
Anxiety—all or most of the time—or panic attacks
Racing, scary thoughts
Feeling guilty or worthless; blaming yourself
Excessive irritability, anger, or agitation; mood swings
Sadness, crying uncontrollably for very long periods of time
Fear of not being a good mother
Fear of being left alone with the baby
Inability to sleep, sleeping too much, difficulty falling or staying asleep
Disinterest in the baby, family, and friends
Difficulty concentrating, remembering details, or making decisions
Thoughts of hurting yourself or the baby (see below for numbers to call to get immediate help).
If these warning signs or symptoms last longer than 2 weeks, you may need to get help. Whether your symptoms are mild or severe, recovery is possible with proper treatment.
What are the risk factors for PPD?
A change in hormone levels after childbirth
Previous experience of depression or anxiety
Family history of depression or mental illness
Stress involved in caring for a newborn and managing new life changes
Having a challenging baby who cries more than usual, is hard to comfort, or whose sleep and hunger needs are irregular and hard to predict
Having a baby with special needs (premature birth, medical complications, illness)
First-time motherhood, very young motherhood, or older motherhood
Other emotional stressors, such as the death of a loved one or family problems
Financial or employment problems
Isolation and lack of social support
What can I do?
Don’t face PPD alone. To find a psychologist or other licensed mental health provider near you, ask your OB/GYN, pediatrician, midwife, internist, or other primary health care provider for a referral. APA can also help you find a local psychologist: Call 1-800-964-2000, or visit the APA Psychologist Locator .
Talk openly about your feelings with your partner, other mothers, friends, and relatives.
Join a support group for mothers—ask your health care provider for suggestions if you can’t find one.
Find a relative or close friend who can help you take care of the baby.
Get as much sleep or rest as you can even if you have to ask for more help with the baby—if you can’t rest even when you want to, tell your primary health care provider.
As soon as your doctor or other primary health care provider says it’s okay, take walks, or participate in another form of exercise.
Try not to worry about unimportant tasks. Be realistic about what you can do while taking care of a new baby.
Cut down on less important responsibilities.
Remember that postpartum depression is not your fault—it is a real, but treatable, psychological disorder. If you are having thoughts of hurting yourself or your baby, take action now: Put the baby in a safe place, like a crib. Call a friend or family member for help if you need to. Then, call a suicide hotline (free and staffed all day, every day):
IMAlive 1-800-SUICIDE (1-800-784-2433)
988 Suicide and Crisis Lifeline Dial 988 (Formerly known as The National Suicide Prevention Lifeline 1-800-273-TALK)
Other versions
Download this Brochure (PDF, 476KB)
En Español (PDF, 419KB)
En Français (PDF, 240KB)
中文 (PDF, 513KB)
All translations of the English Postpartum Depression brochure were partially funded by a grant from the American Psychological Foundation.
Crisis hotlines and resources
Postpartum Health Alliance
Postpartum Support International
American Foundation for Suicide Prevention
Health Resources and Services Administration
National Women’s Health Center
- Psychology topics: Women and girls
- Psychology topics: Depression
You may also like
Postpartum Depression: Treatment and Therapy Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Postpartum depression.
Although for many people the birth of a child is an exciting part of life, for some it may cause adverse health outcomes. One of them is postpartum depression that can be characterized by mood swings, sleep deprivation, and anxiety. This paper discusses a patient that presented in the clinic with these symptoms. It outlines the possible treatment and therapy methods, as well as the implications of the condition.
A 28-year-old patient presented in the office three weeks after giving birth to her first son with the symptoms of postpartum depression. The woman was a single mother; she did not have a strong support system as her former partner refused to help her and her family lived in a different state. She noted that she was sleep-deprived, she felt apathetic, sad, experienced anxiety, and had a decreased appetite.
The patient reported that she was diagnosed with depression seven years ago but underwent treatment and had not had the symptoms for a long time. The woman noted that her mother also had signs of a mental disorder but never sought professional help. The patient cried while talking to me; her emotional state was poor. In addition, the woman admitted that she had thought of harming her newborn son because she felt that she was tired of taking care of him.
The typical signs of postpartum depression include the presence of sleep disorder, fatigue, crying, anxiety, changes in appetite, and feelings of inadequacy (Tharpe, Farley, & Jordan, 2017). The patient has these symptoms, which allowed for establishing the diagnosis. Drug therapy included the prescription of tricyclic antidepressants, as they do not pose risks to infants during breastfeeding (Anxiety and Depression Association of America, 2018). Additional therapies included adequate nutrition with the exclusion of caffeine and herbal remedies, such as 2 cups of lemon balm tea daily (Tharpe et al., 2017).
Moreover, I advised the woman to participate in support groups’ meetings and have a scheduled time for personal care, hobbies, and favorite activities, as well as sleep. In addition, I asked the patient to try to have some time away from her child as it could improve her mental state as well. As for follow-up care measures, I suggested that the woman could document her thoughts and feelings and update me on the changes in her condition by visiting my office in two weeks. Moreover, I invited the patient to participate in an educational session on the aspects of postpartum depression.
The primary implication of the woman’s condition is that it is vital to educate individuals on its symptoms and assure them that this experience is common. Moreover, it is necessary to continue establishing support groups and psychotherapy sessions aimed to eliminate this issue. Postpartum depression may affect not only this woman but her entire family unit as the individuals close to the patient can also start experiencing emotional distress and other related symptoms. In the case of my patient, the condition may affect her relationships with her child, potentially causing a poor emotional bond and behavioral problems in the infant.
Postpartum depression is a severe condition that may affect a patient’s life significantly. It can cause individuals to feel anxious, experience mood swings and changes in appetite, and have thoughts of harming their newborn children. The management strategy for this illness can include drug therapy along with alternative remedies. It is vital to establish support groups and educational training for people having postpartum depression to decrease its incidence.
Anxiety and Depression Association of America. (2018). Postpartum depression . Web.
Tharpe, N. L., Farley, C., & Jordan, R. G. (2017). Clinical practice guidelines for midwifery & women’s health (5th ed.). Burlington, MA: Jones & Bartlett Publishers.
- Dame Stephanie Shirley's Psychological Adjustments
- Dimensions of Psychology and Its Specialty Areas
- Postpartum Depression and Acute Depressive Symptoms
- Supporting the Health Needs of Patients With Parkinson’s, Preeclampsia, and Postpartum Depression
- Technology to Fight Postpartum Depression in African American Women
- Anxiety Disorder: Psychological Studies Comparison
- Mental Illness With Mass Shootings
- A Review of Postpartum Depression and Continued Post Birth Support
- Role of Behavioral Science in Treatment of Dyslexia and Dyscalculia
- The Psychological and Social Problems in Students
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, July 9). Postpartum Depression: Treatment and Therapy. https://ivypanda.com/essays/postpartum-depression-discussion/
"Postpartum Depression: Treatment and Therapy." IvyPanda , 9 July 2021, ivypanda.com/essays/postpartum-depression-discussion/.
IvyPanda . (2021) 'Postpartum Depression: Treatment and Therapy'. 9 July.
IvyPanda . 2021. "Postpartum Depression: Treatment and Therapy." July 9, 2021. https://ivypanda.com/essays/postpartum-depression-discussion/.
1. IvyPanda . "Postpartum Depression: Treatment and Therapy." July 9, 2021. https://ivypanda.com/essays/postpartum-depression-discussion/.
Bibliography
IvyPanda . "Postpartum Depression: Treatment and Therapy." July 9, 2021. https://ivypanda.com/essays/postpartum-depression-discussion/.
Academic Support for Nursing Students
No notifications.
Disclaimer: This essay has been written by a student and not our expert nursing writers. View professional sample essays here.
View full disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this essay are those of the author and do not necessarily reflect the views of NursingAnswers.net. This essay should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
Postpartum Depression: An Important Issue In Women’s Health
Info: 2066 words (8 pages) Nursing Essay Published: 29th May 2020
Reference this
Tagged: mental health depression PPD
If you need assistance with writing your nursing essay, our professional nursing essay writing service is here to help!
Our nursing and healthcare experts are ready and waiting to assist with any writing project you may have, from simple essay plans, through to full nursing dissertations.
- Hantsoo, Liisa, et al. “A Randomized, Placebo-Controlled, Double-Blind Trial of Sertraline for Postpartum Depression.” SpringerLink , Springer Berlin Heidelberg, 31 Oct. 2014, link.springer.com/article/10.1007/s00213-013-3316-1.
- Hyland, Kristina. “Postpartum Depression Research Paper.” LinkedIn SlideShare , 15 Nov. 2015, www.slideshare.net/KristinaHyland/postpartum-depression-research-paper-55121451.
- National Institute of Mental Health, www.nimh.nih.gov/health/publications/postpartum-depression-facts/index.shtmlTables.
- “Postnatal Depression Has Life-Long Impact on Mother-Child Relations.” ScienceDaily , ScienceDaily, 20 Feb. 2018, www.sciencedaily.com/releases/2018/02/180220122917.htm.
- “Postpartum Depression.” Mayo Clinic , Mayo Foundation for Medical Education and Research, 1 Sept. 2018, www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services

- Nursing Essay Writing Service

- Nursing Dissertation Service

- Reflective Writing Service
Related Content
Content relating to: "PPD"
Post-partum or post-natal depression (PPD) affects around 10-15% of mothers having their first baby. Depression during this time is seen as putting the mother at risk for the onset of a serious chronic mood disorder. Symptoms can initially include irritability, tearfulness, insomnia, hypochondriasis, headache and impairment of concentration.
Related Articles

Abstract The purpose of this paper is to educate and inform the audience of a condition known as Postpartum depression (PPD). Throughout this text I will be identifying what exactly PPD is, causes and...
Reflection on Pregnancy and Childbirth
Explain Why the Critical Factors Influencing the Course of Pregnancy Including Several Dimensions such as Social, Biological and Psychological Factors The period in the uterus before conception is a...
Intervention Strategies for Post Partum Depression
More than 1 in 10 women in the United Kingdom develop a mental illness during pregnancy or in the first year after giving birth, according to research by the Centre for Mental Health and London ...
DMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on the NursingAnswers.net website then please:
Our academic writing and marking services can help you!
- Marking Service
- Samples of our Work
- Full Service Portfolio
Related Lectures
Study for free with our range of nursing lectures!
- Drug Classification
- Emergency Care
- Health Observation
- Palliative Care
- Professional Values

Write for Us
Do you have a 2:1 degree or higher in nursing or healthcare?
Study Resources
Free resources to assist you with your nursing studies!
- APA Citation Tool
- Example Nursing Essays
- Example Nursing Assignments
- Example Nursing Case Studies
- Reflective Nursing Essays
- Nursing Literature Reviews
- Free Resources
- Reflective Model Guides
- Nursing and Healthcare Pay 2021

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- U.S. Department of Health & Human Services

Call the OWH HELPLINE: 1-800-994-9662 9 a.m. — 6 p.m. ET, Monday — Friday OWH and the OWH helpline do not see patients and are unable to: diagnose your medical condition; provide treatment; prescribe medication; or refer you to specialists. The OWH helpline is a resource line. The OWH helpline does not provide medical advice.
Please call 911 or go to the nearest emergency room if you are experiencing a medical emergency.
Postpartum depression

Your body and mind go through many changes during and after pregnancy. If you feel sad, anxious, or overwhelmed or feel like you don’t love or care for your baby and these feelings last longer than 2 weeks during or after pregnancy, you may have postpartum depression. Treatment for depression, such as therapy or medicine, works and can help you and your baby be as healthy as possible in the future.
What is postpartum depression?
“Postpartum” means the time after having a baby. Some women get the “baby blues,” or feel sad, worried, or tired within a few days of giving birth. For many women, the baby blues go away in a few days. If these feelings don’t go away or you feel sad, hopeless, or anxious for longer than 2 weeks, you may have postpartum depression. Feeling hopeless after childbirth is not a regular or expected part of being a mother.
Postpartum depression is a serious mental health condition that involves the brain and affects your behavior and physical health. If you have depression, then sad and hopeless feelings don’t go away and can interfere with your day-to-day life. You might not feel connected to your baby, as if you are not the baby’s mother, or you might not love or care for the baby. These feelings can be mild to severe.
Mothers can also experience anxiety disorders during or after pregnancy.
How common is postpartum depression?
Depression is a common problem after pregnancy . One in 8 new mothers report experiencing symptoms of postpartum depression in the year after childbirth. 1
How do I know if I have postpartum depression?
Some normal changes after pregnancy can cause symptoms similar to those of depression. Many mothers feel overwhelmed when a new baby comes home. But if you have any of the following symptoms of depression for more than 2 weeks, call your doctor, nurse, or midwife:
- Feeling angry or moody
- Feeling sad or hopeless
- Feeling guilty, shameful, or worthless
- Eating more or less than usual
- Sleeping more or less than usual
- Unusual crying or sadness
- Loss of interest, joy, or pleasure in thing you used to enjoy
- Withdrawing from friends and family
- Possible thoughts of harming the baby or yourself
Some women don’t tell anyone about their symptoms. New mothers may feel embarrassed, ashamed, or guilty about feeling depressed when they are supposed to be happy. They may also worry they will be seen as bad mothers. Any woman can become depressed during pregnancy or after having a baby. It doesn’t mean you are a bad mom. You don’t have to suffer. There is help. Your doctor can help you figure out whether your symptoms are caused by depression or something else.
What causes postpartum depression?
The exact cause of PPD is not known and many different factors are likely to contribute to someone developing PPD. Hormonal changes may trigger symptoms of postpartum depression. When you are pregnant, levels of the female hormones estrogen and progesterone are the highest they’ll ever be. In the first 24 hours after childbirth, hormone levels quickly drop back to normal, pre-pregnancy levels. Researchers think this sudden change in hormone levels may lead to depression . 2 This is similar to hormone changes before a woman’s period but involves much more extreme swings in hormone levels.
Levels of thyroid hormones may also drop after giving birth. The thyroid is a small gland in the neck that helps regulate how your body uses and stores energy from food. Low levels of thyroid hormones can cause symptoms of depression. A simple blood test can tell whether this condition is causing your symptoms. If so, your doctor can prescribe thyroid medicine.
Are some women more at risk of postpartum depression?
Yes. You may be more at risk of postpartum depression if you:
- Had depression before or during pregnancy
- Have a family history of depression
- Experienced abuse or adversity as a child
- Had a difficult or traumatic birth
- Had problems with a previous pregnancy or birth
- Have little or no support from family, friends, or partners
- If you are now or have experienced domestic violence
- Have relationship struggles, money problems, or experience other stressful life events
- Are under the age of 20
- Have a hard time breastfeeding
- Have a baby that was born prematurely and/or has special health care needs
- Had an unplanned pregnancy
The U.S. Preventive Services Task Force recommends that doctors look for and ask about symptoms of depression during and after pregnancy, regardless of a woman’s risk of depression. 4
What is the difference between “baby blues” and postpartum depression?
Many women have the baby blues in the days after childbirth. If you have the baby blues, you may:
- Have mood swings
- Feel sad, anxious, or overwhelmed
- Have crying spells
- Lose your appetite
- Have trouble sleeping
The baby blues usually go away within a few days. The symptoms of postpartum depression last longer, are more severe, and may require treatment by a health care professional. Postpartum depression usually begins within the first month after birth.
What should I do if I have symptoms of postpartum depression?
Call your doctor, nurse, midwife, or pediatrician if:
- Your baby blues symptoms don’t go away after 2 weeks or are very intense
- Symptoms of depression begin within 1 year of delivery and last more than 2 weeks
- It is difficult to work or get things done at home
- You cannot care for yourself or your baby (e.g., eating, sleeping, bathing)
- You have thoughts about hurting yourself or your baby
Ask your partner or a loved one to call for you if necessary. Your doctor, nurse, or midwife can ask you questions to test for depression. They can also refer you to a mental health professional for help and treatment.
What can I do at home to feel better while seeing a doctor for postpartum depression?
Here are some ways to begin feeling better or getting more rest, in addition to talking to a health care professional:
- Rest as much as you can. Sleep when the baby is sleeping.
- Don’t try to do too much or to do everything by yourself. Ask your partner, family, and friends for help.
- Make time to go out, visit friends, or spend time alone with your partner.
- Talk about your feelings with your partner, supportive family members, and friends.
- Talk with other mothers so that you can learn from their experiences.
- Join a support group. Ask your doctor or nurse about groups in your area.
- Don’t make any major life changes right after giving birth. More major life changes in addition to a new baby can cause unneeded stress. Sometimes big changes can’t be avoided. When that happens, try to arrange support and help in your new situation ahead of time.
It can also help to have a partner, a friend, or another caregiver who can help take care of the baby while you are depressed. If you are feeling depressed during pregnancy or after having a baby, don’t suffer alone. Tell a loved one and call your doctor right away.
How is postpartum depression treated?
Working with a health care professional is a good way to create a plan that will work for you. Here are some ways to get help—they can be used alone or together:
- Therapy: Counseling or therapy sessions with a mental health professional can help you understand and cope with your emotions and challenges.
- Support groups: Joining a support group of others experiencing PPD can provide comfort and understanding.
- Self-care: Taking care of yourself is important. Do your best to get enough rest, eat food with a lot of nutrients like fresh produce and whole grains, be physically active, and ask for help when needed.
- Social support: Reach out to family, friends, or other people you trust who can offer advice or support.
- Medication: In some cases, medicine may be prescribed to help manage symptoms. The most common type is antidepressants. Antidepressants can help relieve symptoms of depression and some can be taken while you're breastfeeding. Antidepressants may take several weeks to start working.
- The Food and Drug Administration (FDA) has also approved a medicine called brexanolone to treat postpartum depression in adult women . 6 Brexanolone is given by a doctor or nurse through an IV for 2½ days (60 hours). Because of the risk of side effects, this medicine can only be given in a clinic or office while you are under the care of a doctor or nurse. Brexanolone may not be safe to take while pregnant or breastfeeding. Zuranolone, the first oral medication approved to treat postpartum depression may be another option.
These treatments can be used alone or together. Talk with your doctor or nurse about the benefits and risks of taking medicine to treat depression when you are pregnant or breastfeeding.
Having depression can affect your baby. Getting treatment is important for you and your baby. Getting help is a sign of strength.
What can happen if postpartum depression is not treated?
Untreated postpartum depression can affect your ability to parent. You may:
- Not have enough energy
- Have trouble focusing on the baby's needs and your own needs
- Not be able to care for your baby
- Have a higher risk of attempting suicide
Feeling bad about yourself can make depression worse. It is important to reach out for help if you feel depressed .
Researchers believe postpartum depression in a mother can affect the healthy development of her child which can cause: 7
- Delays in language development and problems learning
- Problems with mother-child bonding
- Behavior problems
- More crying or agitation
- Shorter height 8 and higher risk of obesity in pre-schoolers 9
- Problems dealing with stress and adjusting to school and other social situations 10
Did we answer your question about postpartum depression?
The resources below can help you learn more about PPD and can guide you in finding additional help.
- Call or text the Suicide and Crisis Lifeline at 988 for free access to a trained crisis counselor who can provide you with support and connect you with additional help and resources. If you’re deaf or hard of hearing, use your preferred relay service or dial 711 then 988 .
- Call or text the National Maternal Mental Health Hotline at 1-833-TLC-MAMA ( 1-833-852-6262 ) for 24/7 free access to professional counselors. If you’re deaf or hard of hearing, use your preferred relay service or dial 711 then 1-833-852-6262 .
- Call or text “Help” to the Postpartum Support International helpline at 1-800-944-4773 for PPD information, resources, and support groups for women, partners, and supporters.
- Ask a health care professional or find a local health center.
- Reach out to local organizations like social service agencies, family resource centers, libraries, community centers, or places of worship.
- Look for support groups in your area, such as new moms’ groups, breastfeeding support groups, or a baby café. See if there are mother/baby exercise programs in your community.
- Centers for Disease Control and Prevention, Division of Reproductive Health. (2020). Pregnancy Risk Assessment Monitoring System (PRAMS). Washington, DC: Centers for Disease Control and Prevention. Retrieved from: https://www.cdc.gov/prams/prams-data/mch-indicators/states/pdf/2020/All-Sites-PRAMS-MCH-Indicators-508.pdf . Accessed on June 5th, 2023.
- Schiller, C.E., Meltzer-Brody, S., Rubinow, D.R. (2014). The Role of Reproductive Hormones in Postpartum Depression . CNS Spectrums; 20(1): 48–59.
- Sit, D.K., Wisner, K.L. (2009). The Identification of Postpartum Depression . Clinical Obstetrics and Gynecology; 52(3): 456–468.
- U.S. Preventive Services Task Force. (2016). Depression in Adults: Screening .
- Alhusen, J.L., Alvarez, C. (2016). Perinatal depression . The Nurse Practitioner; 41(5): 50–55.
- U.S. Food and Drug Administration. (2019). FDA approves first treatment for post-partum depression .
- Stein, A., Perason, R.M., Goodman, S.H., Rapa, E., Rahman, A., McCallum, M., et al. (2014). Effects of perinatal mental disorders on the fetus and child . Lancet; 384(9956): 1800–1819.
- Surkan, P.J., Ettinger, A.K., Hock, R.S., Ahmed, S., Strobino, D.M., Minkovitz, C.S. (2014). Early maternal depressive symptoms and child growth trajectories: a longitudinal analysis of a nationally representative US birth cohort . BMC Pediatrics; 14: 185.
- Benton, P.M., Skouteris, H., Hayden, M. (2015). Does maternal psychopathology increase the risk of pre-schooler obesity? A systematic review . Appetite; 87(1): 259–282.
- Korhonen, M., Luoma, I., Salmelin, R., Tamminen, T. (2014). Maternal depressive symptoms: Associations with adolescents' internalizing and externalizing problems and social competence . Nordic Journal of Psychiatry; 68(5): 323–332.
To learn more about postpartum depression and access educational resources, visit our Talking Postpartum Depression campaign page.
- HHS Non-Discrimination Notice
- Language Assistance Available
- Accessibility
- Privacy Policy
- Disclaimers
- Freedom of Information Act (FOIA)
- Use Our Content
- Vulnerability Disclosure Policy
- Kreyòl Ayisyen
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
1101 Wootton Pkwy, Rockville, MD 20852 1-800-994-9662 • Monday through Friday, 9 a.m. to 6 p.m. ET (closed on federal holidays).

Home — Essay Samples — Nursing & Health — Neurology & Nervous System Diseases — Postpartum Depression
Essay Examples on Postpartum Depression
Depression: an informative exploration, postpartum depression and anxiety disorders in women, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Suffering in Silence: The Development of Postpartum Depression
Jane's postpartum depression in the yellow wallpaper by charlotte perkins gilman, the factors of postpartum depression, the effects of postpartum depression in the poem the yellow wallpaper by charlotte perkins gilman, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Postpartum Depression Among Canadian Women
Bond between mother and child: postpartum depression in immigrants, relevant topics.
- Post Traumatic Stress Disorder
- Sleep Deprivation
- Drug Addiction
- Stress Management
- Healthy Food
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Patient Care & Health Information
- Diseases & Conditions
- Postpartum depression
The birth of a baby can start a variety of powerful emotions, from excitement and joy to fear and anxiety. But it can also result in something you might not expect — depression.
Most new moms experience postpartum "baby blues" after childbirth, which commonly include mood swings, crying spells, anxiety and difficulty sleeping. Baby blues usually begin within the first 2 to 3 days after delivery and may last for up to two weeks.
But some new moms experience a more severe, long-lasting form of depression known as postpartum depression. Sometimes it's called peripartum depression because it can start during pregnancy and continue after childbirth. Rarely, an extreme mood disorder called postpartum psychosis also may develop after childbirth.
Postpartum depression is not a character flaw or a weakness. Sometimes it's simply a complication of giving birth. If you have postpartum depression, prompt treatment can help you manage your symptoms and help you bond with your baby.
Products & Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- A Book: Mayo Clinic Guide to Your Baby's First Years
Symptoms of depression after childbirth vary, and they can range from mild to severe.
Baby blues symptoms
Symptoms of baby blues — which last only a few days to a week or two after your baby is born — may include:
- Mood swings
- Irritability
- Feeling overwhelmed
- Reduced concentration
- Appetite problems
- Trouble sleeping
Postpartum depression symptoms
Postpartum depression may be mistaken for baby blues at first — but the symptoms are more intense and last longer. These may eventually interfere with your ability to care for your baby and handle other daily tasks. Symptoms usually develop within the first few weeks after giving birth. But they may begin earlier — during pregnancy — or later — up to a year after birth.
Postpartum depression symptoms may include:
- Depressed mood or severe mood swings
- Crying too much
- Difficulty bonding with your baby
- Withdrawing from family and friends
- Loss of appetite or eating much more than usual
- Inability to sleep, called insomnia, or sleeping too much
- Overwhelming tiredness or loss of energy
- Less interest and pleasure in activities you used to enjoy
- Intense irritability and anger
- Fear that you're not a good mother
- Hopelessness
- Feelings of worthlessness, shame, guilt or inadequacy
- Reduced ability to think clearly, concentrate or make decisions
- Restlessness
- Severe anxiety and panic attacks
- Thoughts of harming yourself or your baby
- Recurring thoughts of death or suicide
Untreated, postpartum depression may last for many months or longer.
Postpartum psychosis
With postpartum psychosis — a rare condition that usually develops within the first week after delivery — the symptoms are severe. Symptoms may include:
- Feeling confused and lost
- Having obsessive thoughts about your baby
- Hallucinating and having delusions
- Having sleep problems
- Having too much energy and feeling upset
- Feeling paranoid
- Making attempts to harm yourself or your baby
Postpartum psychosis may lead to life-threatening thoughts or behaviors and requires immediate treatment.
Postpartum depression in the other parent
Studies show that new fathers can experience postpartum depression, too. They may feel sad, tired, overwhelmed, anxious, or have changes in their usual eating and sleeping patterns. These are the same symptoms that mothers with postpartum depression experience.
Fathers who are young, have a history of depression, experience relationship problems or are struggling financially are most at risk of postpartum depression. Postpartum depression in fathers — sometimes called paternal postpartum depression — can have the same negative effect on partner relationships and child development as postpartum depression in mothers can.
If you're a partner of a new mother and are having symptoms of depression or anxiety during your partner's pregnancy or after your child's birth, talk to your health care provider. Similar treatments and supports provided to mothers with postpartum depression can help treat postpartum depression in the other parent.
When to see a doctor
If you're feeling depressed after your baby's birth, you may be reluctant or embarrassed to admit it. But if you experience any symptoms of postpartum baby blues or postpartum depression, call your primary health care provider or your obstetrician or gynecologist and schedule an appointment. If you have symptoms that suggest you may have postpartum psychosis, get help immediately.
It's important to call your provider as soon as possible if the symptoms of depression have any of these features:
- Don't fade after two weeks.
- Are getting worse.
- Make it hard for you to care for your baby.
- Make it hard to complete everyday tasks.
- Include thoughts of harming yourself or your baby.
If you have suicidal thoughts
If at any point you have thoughts of harming yourself or your baby, immediately seek help from your partner or loved ones in taking care of your baby. Call 911 or your local emergency assistance number to get help.
Also consider these options if you're having suicidal thoughts:
- Seek help from a health care provider.
- Call a mental health provider.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential. The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Helping a friend or loved one
People with depression may not recognize or admit that they're depressed. They may not be aware of signs and symptoms of depression. If you suspect that a friend or loved one has postpartum depression or is developing postpartum psychosis, help them seek medical attention immediately. Don't wait and hope for improvement.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
There is no single cause of postpartum depression, but genetics, physical changes and emotional issues may play a role.
- Genetics. Studies show that having a family history of postpartum depression — especially if it was major — increases the risk of experiencing postpartum depression.
- Physical changes. After childbirth, a dramatic drop in the hormones estrogen and progesterone in your body may contribute to postpartum depression. Other hormones produced by your thyroid gland also may drop sharply — which can leave you feeling tired, sluggish and depressed.
- Emotional issues. When you're sleep deprived and overwhelmed, you may have trouble handling even minor problems. You may be anxious about your ability to care for a newborn. You may feel less attractive, struggle with your sense of identity or feel that you've lost control over your life. Any of these issues can contribute to postpartum depression.
Risk factors
Any new mom can experience postpartum depression and it can develop after the birth of any child, not just the first. However, your risk increases if:
- You have a history of depression, either during pregnancy or at other times.
- You have bipolar disorder.
- You had postpartum depression after a previous pregnancy.
- You have family members who've had depression or other mood disorders.
- You've experienced stressful events during the past year, such as pregnancy complications, illness or job loss.
- Your baby has health problems or other special needs.
- You have twins, triplets or other multiple births.
- You have difficulty breastfeeding.
- You're having problems in your relationship with your spouse or partner.
- You have a weak support system.
- You have financial problems.
- The pregnancy was unplanned or unwanted.
Complications
Left untreated, postpartum depression can interfere with mother-child bonding and cause family problems.
- For mothers. Untreated postpartum depression can last for months or longer, sometimes becoming an ongoing depressive disorder. Mothers may stop breastfeeding, have problems bonding with and caring for their infants, and be at increased risk of suicide. Even when treated, postpartum depression increases a woman's risk of future episodes of major depression.
- For the other parent. Postpartum depression can have a ripple effect, causing emotional strain for everyone close to a new baby. When a new mother is depressed, the risk of depression in the baby's other parent may also increase. And these other parents may already have an increased risk of depression, whether or not their partner is affected.
- For children. Children of mothers who have untreated postpartum depression are more likely to have emotional and behavioral problems, such as sleeping and eating difficulties, crying too much, and delays in language development.
If you have a history of depression — especially postpartum depression — tell your health care provider if you're planning on becoming pregnant or as soon as you find out you're pregnant.
- During pregnancy, your provider can monitor you closely for symptoms of depression. You may complete a depression-screening questionnaire during your pregnancy and after delivery. Sometimes mild depression can be managed with support groups, counseling or other therapies. In other cases, antidepressants may be recommended — even during pregnancy.
- After your baby is born, your provider may recommend an early postpartum checkup to screen for symptoms of postpartum depression. The earlier it's found, the earlier treatment can begin. If you have a history of postpartum depression, your provider may recommend antidepressant treatment or talk therapy immediately after delivery. Most antidepressants are safe to take while breastfeeding.
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision DSM-5-TR. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed May 9, 2022.
- Postpartum depression. Office on Women's Health. https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression. Accessed May 5, 2022.
- Depression among women. Centers for Disease Control and Prevention. https://www.cdc.gov/reproductivehealth/depression/index.htm. Accessed May 5, 2022.
- What is peripartum depression (formerly postpartum)? American Psychiatric Association. https://www.psychiatry.org/patients-families/postpartum-depression/what-is-postpartum-depression. Accessed Nov. 18, 2022.
- Viguera A. Postpartum unipolar depression: Epidemiology, clinical features, assessment, and diagnosis. https://www.uptodate.com/contents/search. Accessed Nov. 18, 2022.
- Viguera A. Mild to moderate postpartum unipolar major depression: Treatment. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Viguera A. Severe postpartum unipolar major depression: Choosing treatment. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Faden J, et al. Intravenous brexanolone for postpartum depression: What it is, how well does it work, and will it be used? Therapeutic Advances in Psychopharmacology. 2020; doi:10.1177/2045125320968658.
- FAQs. Postpartum depression. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/postpartum-depression. Accessed May 6, 2022.
- Suicide prevention. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/suicide-prevention. Accessed May 6, 2022.
- Postpartum depression. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/postpartum-depression#. Accessed May 6, 2022.
- AskMayoExpert. Depression in pregnancy and postpartum. Mayo Clinic; 2022.
- American Academy of Pediatrics. Postpartum care of the mother. In: Guidelines for Perinatal Care. 8th ed. American Academy of Pediatrics; American College of Obstetricians and Gynecologists; 2017.
- Kumar SV, et al. Promoting postpartum mental health in fathers: Recommendations for nurse practitioners. American Journal of Men's Health. 2018; doi:10.1177/1557988317744712.
- Scarff JR. Postpartum depression in men. Innovations in Clinical Neuroscience. 2019;16:11.
- Bergink V, et al. Postpartum psychosis: Madness, mania, and melancholia in motherhood. American Journal of Psychiatry. 2016; doi:10.1176/appi.ajp.2016.16040454.
- Yogman M, et al. Fathers' roles in the care and development of their children: The role of pediatricians. Pediatrics. 2016; doi:10.1542/peds.2016-1128.
- FDA approves first treatment for post-partum depression. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-post-partum-depression. Accessed May 6, 2022.
- Deligiannidis KM, et al. Effect of zuranolone vs placebo in postpartum depression: A randomized clinical trial. JAMA Psychiatry. 2021; doi:10.1001/jamapsychiatry.2021.1559.
- Betcher KM (expert opinion). Mayo Clinic. May 10, 2022.
- 988 Suicide & Crisis Lifeline. https://988lifeline.org/. Accessed Nov. 18, 2022.
Associated Procedures
- Electroconvulsive therapy (ECT)

News from Mayo Clinic
- Mayo Clinic Minute: Postpartum depression is more than baby blues Feb. 02, 2023, 03:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
ORIGINAL RESEARCH article
A comprehensive analysis of post-partum depression risk factors: the role of socio-demographic, individual, relational, and delivery characteristics.

- 1 Department of Surgical, Medical and Molecular Pathology and Critical Care Medicine, University of Pisa, Pisa, Italy
- 2 Department of Educations, Languages, Intercultures, Literatures and Psychology, University of Florence, Florence, Italy
- 3 Division of Obstetrics and Gynaecology, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Postpartum depression is a common and complex phenomenon that can cause relevant negative outcomes for children, women and families. Existing literature highlights a wide range of risk factors. The main focus of this paper is to jointly investigate different types of risk factors (socio-demographic, psychopathological, relational, and related to labor and birth experience) in post-partum depression onset in women during first-child pregnancy, identifying which of these are the most important predictors. A cohort longitudinal study was conducted on 161 Italian nulliparous low-risk women ( M age = 31.63; SD = 4.88) without elective cesarean. Data was collected at three different times: Socio-demographic, prenatal anxiety and depression, and quality of close relationship network (with mother, father and partner, and the prenatal attachment to child) were assessed at T1 (week 31–32 of gestation); clinical data on labor and childbirth (mode and typology of delivery, duration of labor, duration of eventual administration of epidural analgesia, and child's APGAR index at birth) were registered at T2 (the day of childbirth); and the degree of post-natal depression symptomatology was measured at T3 (1 month after birth). Postpartum depression is associated with several risk factors (woman's age, woman's prenatal psychopathological characteristics, the level of prenatal attachment to child, the quality of romantic relationship, and some clinical delivery difficulties). Overall, the level of prenatal attachment to child was the most important predictor of post-partum depression. These findings emphasize the very important role of prenatal attachment for the onset of postpartum depression and the need to promote adequate and targeted prevention interventions. Limitations, strengths, and theoretical and clinical implications are discussed.
Introduction
For a woman, the gestation of her first child has been identified as a central life event ( 1 ). From a psychological perspective, in fact, the pregnancy of the first baby involves the transition to motherhood, a major developmental period with important implications for mothers, for the infant-mother relationship, and the infant's development ( 2 ). During the first pregnancy, a woman's maternal identity develops through the reorganization of mental self-representation and the elaboration of other significant relationships ( 3 , 4 ). The woman's mental self-representation enriches with the maternal component, thus leading her to review the relationship with her own mother; the mental couple image gradually modifies with integration of the family image, and the marital relationship is reorganized with the parental component. With the birth of the first child, the quality of the couple relationship may undergo temporary changes that are influenced by the ability of the parents to adapt to new needs ( 5 ).
The transition to parenthood (transition to parenthood—TTP) has often been associated with marital crisis, and the premise in literature was that parenthood creates serious individual and relationship distress ( 6 , 7 ). Parenting can be an improvement factor for some couple relationships; however, it can also be disruptive and increase problems ( 8 ). While some couples may develop new skills in resolving difficulties, others find themselves running aground trying to develop these skills ( 6 ).
All the above physical, psychological, and relational changes that occur during the perinatal period may increase the risk for maternal emotional vulnerability, such as depressed emotions. The DSM-5 proposes the term “peripartum onset” as a major depressive episode during pregnancy or in the weeks or months following delivery ( 9 ). This condition is characterized by sad mood, anxiety, irritability, lack of positive emotions, loss of pleasure, interests and energy, decreased appetite, inability to cope, fear of hurting self and baby, and suicidal thoughts ( 10 , 11 ). Both anxiety and depression can occur in the perinatal period (up to 1 year after delivery) ( 9 ) and these conditions present high rates of co-morbidity ( 12 ). The first weeks immediately after childbirth are the most critical ( 13 ), and although the increased vulnerability continues for the following 6 months ( 14 – 16 ), post-partum depression (PPD) generally occurs within the first month after delivery ( 9 ).
This vulnerability is higher for primiparous mothers, who present an increased risk for depression in the postpartum period ( 12 , 17 , 18 ), especially in the first 90 days after delivery ( 19 ). Although contrasting results emerged about the prevalence of postpartum depression in relation to parity ( 20 , 21 ), studies conducted in the European context showed that the prevalence for PPD in primiparas was 11.8 vs. 8.6% in multiparas ( 21 ).
In fact, maternal inexperience leads new mothers to have greater difficulty in early interactions with their children, and research has reported that the effect of maternal depression is greater in nulliparas compared to multiparas ( 22 ).
Although from a psychiatric perspective postpartum depression is no longer classified as a distinct entity, from a psychological perspective, depression occurring during the postpartum period has particular relevance in a woman's life.
In fact, it enhances the risk of a multitude of negative consequences for children, women, and families, including poor infant physical health and more frequent sickness, and physiological, psychological, emotional, and psychomotor delays during infancy and early childhood ( 23 ).
Moreover, PPD can negatively affect the ability and the availability of women to adequately take care of their children. Henderson et al. ( 24 ) have shown the important negative outcomes that PPD can have on mother-infant interactions, the child's growth, and the tendency to quit breastfeeding earlier. Moreover, children of mothers with PPD tend to establish insecure attachment bonds and develop social difficulties with peers ( 25 , 26 ).
Because of these relevant consequences, it is important to identify the risk factors that can be involved in the development of PPD in first-time mothers.
Several factors, both internal and external, have been found to be related to PPD, and it is plausible that a complex interplay of these can be the cause of greater vulnerability ( 27 ), especially in women during their first pregnancy, compared to those who already have a child. Alongside psychological risk factors, such as a lifetime history of depression, and a presence of antenatal depression and prenatal anxiety ( 28 , 29 ), many authors have shown that relational variables constitute significant risk factors for post-partum depression development. Problems in maternal and romantic relationships, such as marital instability, and low level of maternal ( 30 , 31 ) and marital support ( 32 ) have been found to be linked with PPD. Priel and Besser ( 33 ) have also found that antenatal attachment was closely linked to PPD. A higher level of antenatal attachment to child predicted a lower level of depressive symptomatology after birth. The presence of stressful life events, or the lack of social support from peer and health professionals, can foster the subsequent development of PPD ( 34 – 36 ).
There are other clinical aspects linked to pregnancy and delivery that are associated to the PPD condition. A complicated labor and birth characterized by longer length of labor and greater pain, or medical intervention during delivery, can result in negative consequences, varying from maternal distress to PPD ( 31 , 37 ). Given that the nulliparous tend to be less self-confident in the maternal role, and that being less self-confident has been associated with postpartum depression ( 38 ), labor and delivery complications can be particularly difficult for first-time mothers.
Finally, some socio-demographic characteristics, such as a young age, or low level of education, or low income, may be considered linked to a higher probability of developing PPD ( 39 , 40 ).
Despite the relevance of these risk factors, most studies have focused on psychopathology and social network aspects linked to maternal and romance relationships, and less attention has been directed to the exploration of these factors jointly.
The aims of this study were: (1) to confirm previous results exploring the role that several sets of variables, such as socio-demographic, individual, relational, and related to delivery characteristics, separately considered, play as risk factors for the onset of postpartum depression; and (2) to verify which, among the above risk factors, have a more significant influence when they are considered together.
In accordance with literature, it was hypothesized that: (1) young age, low level of education, low employment status, and not planned pregnancy, could positively predict levels of PPD; (2) prenatal anxiety and depression positively predict PPD; (3) an affectionate prenatal attachment, and a good quality romantic and parental relationship negatively predict PPD; (4) a more complicated labor (in terms of duration and duration of epidural and oxytocin administration), the modality of delivery (cesarean section vs. vaginal birth) and a worse index of newborn well-being (in terms of lower Apgar score) positively predict PPD. No hypotheses were developed about the strongest predictor for PPD.
Materials and Methods
Procedure and participants.
The study was conducted in accordance with the guidelines for the ethical treatment of human participants of the Italian Psychological Association. The Ethical Committee of Azienda USL 4 Prato, Italy, had previously approved the study (no 780/2013). Data were collected during 2014 in the maternity ward of a public hospital of the metropolitan area of Prato (Italy), a unit with about 1,130 deliveries per year (69% Italian women), from January to December 2014, during delivery preparation courses organized for pregnant women (>30 weeks of gestation).
A cohort longitudinal study was carried out. Data were collected at three different time points: (1) 31–32 week of gestation; (2) the day of delivery; and (3) 1 month after childbirth.
Inclusion criteria were: Italian women, age >18 years, physically and psychologically healthy nulliparous women with singleton low-risk pregnancies, gestational age >31 weeks. Exclusion criteria were: twin pregnancy, maternal pathologies during pregnancy, fetal pathologies, the presence of depressive pathologies documented in clinical records, and planned elective cesarean. Planned elective cesarean was an exclusion criterium because we were interested in examining the roles of labor and delivery as predictors of PPD. Therefore, we excluded from the study women who underwent planned elective cesarean, but not those who experienced emergency cesarean after labor.
The participants ( n = 191) were informed about the aims of the study and signed a written informed consent form. They could withdraw from participation at any time. Ninety-four percent of the women who were contacted consented to participate in the survey ( n = 179) and, of them, 90% completed the entire follow-up (Time 1, 2, and 3). At T1 we recruited 179 women, but by T3 we lost 18 women who did not return the completed questionnaire. The final sample consisted of 161 nulliparous pregnant women aged 18–42 years ( M = 31.63, SD = 4.88). Our sample is representative regarding both size and age of the general population of women giving birth in Prato that meet our inclusion criteria.
At time 1, all participants received a battery of questionnaires for the collection of socio-demographic, clinical, psychological and relational data. In particular:
Socio-Demographic and Clinical Measures
Participants provided their age, educational level, work status, marital status, information about the number of years of their couple relationship, and information about planned or not pregnancy.
Psychological Measures
Participants were asked to complete psychological questionnaires to assess psychopathological characteristics. To assess the women's anxiety level, the State Anxiety Inventory (STAI_Y2) ( 41 , 42 ) was used. This questionnaire is the most widely used measure of anxiety during pregnancy, especially in association with postnatal depression ( 43 ). The STAI_Y2 is a 20-item self-report questionnaire asking to report how often the anxiety state was experienced. Responses were rated on a 4-point Likert scale, from 1 (never) to 4 (very often) The total score is obtained by summing all items, after some items are overturned, and can range from 20 to 80. A high score indicates a high level of anxiety. For the current study, Cronbach's alpha was 0.90.
To detect the level of women's depression, the Beck Depression Inventory (BDI) ( 44 , 45 ) was used. The BDI is a 21-item self-report inventory used for measuring the severity of symptoms. Each item had a set of four responses ranging in intensity from 0 to 3. The total score is obtained by summing all items and can range from 0 to 63. High scores indicate high depressive symptomatology. In the present sample, Cronbach's value was 0.84.
Relational Measures
All women were asked to complete four questionnaires assessing the quality of their close relationship network, with their mother, father and partner, and the level of their prenatal attachment to child. In particular, the quality of women's relationships with mothers and fathers was assessed using the Parental Bonding Instrument (PBI) ( 46 , 47 ). The PBI consists of two parallel versions of 21 items, ranging from 0 (Very likely) to 3 (Very unlikely), which assessed three dimensions: Care, Encouragement toward autonomy, and Overprotection. In the present sample, Cronbach's values for the paternal version were 0.98, 0.98, and 0.96 for Care, Encouragement toward autonomy, and Overprotection, respectively. For the maternal version, Cronbach's values for Care, Encouragement toward autonomy, and Overprotection were 0.98, 0.96, and 0.87, respectively. In this study, we used a global dimension of the relationship quality, summing the above three dimensions, according to the procedure described in the results section. The total score for PBI is obtained by summing all items and can range from 0 to 63. High scores on this dimension indicate that the women perceive a good quality of their maternal and paternal relationships.
The quality of the women's romantic relationships was assessed using the Romance Qualities Scale (RQS) ( 48 ). The RQS is a 22-item self-report instrument, ranging from 1 (Absolutely false) to 5 (Absolutely true), which assesses five main qualitative dimensions of the relationship with partner (companionship, conflict, help, security and closeness) and a global score of the romantic relationship quality. The total score is obtained by summing all items and can range from 22 to 110. High scores on this dimension indicate that women perceive a good quality of their romantic relationships. In the present sample, Cronbach's value was 0.84.
The Prenatal Attachment Inventory (PAI) ( 49 , 50 ) was used to measure the mother's attachment bond to her child during pregnancy. The PAI is a self-report questionnaire with 21 items from 1 (Almost never) to 4 (Almost always). The total score is obtained by summing all items and can range from 21 to 84. High scores indicate a good quality of prenatal attachment bond. For the present sample, the Cronbach's alpha was 0.93.
At time 2, clinical information regarding labor, delivery and birth outcomes was extracted from hospital records after childbirth. In particular:
Labor measures including three indices: (a) modality of labor (induced vs. spontaneous); (b) duration of labor in hours; (c) administration of epidural analgesia in hours (no analgesia administration = 0).
Mode of delivery, recorded according to category: vaginal (natural and operative vaginal delivery) vs. emergency cesarean delivery.
Birth outcomes, assessed via APGAR scores at 1 min. APGAR score index at birth was determined by evaluating the newborn baby on: color, heart rate, reflexes, muscle tone, respiration). Scores ≤3 are generally regarded as critically low, 4–6 fairly low, and 7–10 generally normal.
At time 3, women were requested to fill out a psychological questionnaire to assess the degree of postnatal depression symptomatology. Diagnosing depression in post-partum may be particularly challenging due to the overlap of diagnostic depressive symptoms with those of a normal post-partum period for women (e.g., fatigue, decreased libido, and sleep or appetite change). Nevertheless, as documented by several authors, the Edinburgh Postnatal Depression Scale (EPDS) ( 51 , 52 ), originally devised for the identification of postpartum depression disorders, allows us to measure affective aspects rather than physical symptoms of depression that may be affected by the perinatal period ( 52 ). The EPDS is a self-report questionnaire consisting of 10 items ranging from 0 to 3, according to increasing severity of the symptom. The total score is obtained by summing all items and can range from 0 to 30 with higher scores on this scale indicating higher levels of postnatal depression symptomatology. For the current sample, Cronbach's alpha was 0.88.
Data Analysis
Data were analyzed using SPSS version 24 (2017). Frequency, means, standard deviation, and bivariate correlation were calculated for all variables. To determine the relationship between predictor variables and postpartum depression, linear regression analyses were separately undertaken for each set of risk factor variables considered.
Regarding parental relationships, we were interested in creating an aggregate score of the quality of maternal and paternal relationship. To verify the possibility to use a single score for the quality of maternal and paternal relationships to include in the regression analysis, two factorial analyses with the three dimensions of the PBI were conducted, separately for the mother and father versions.
Subsequently, to explore the stronger risk factors, a linear regression (stepwise method) was conducted with post-partum depression as the dependent variable, and the significant risk factors were entered as predictors. An alpha level of 0.05 was used for all statistical tests.
All the women had a middle or high socioeconomic level; 87% had a high school diploma or bachelor's degree (13% of women had a secondary school diploma, 54% had a high school diploma, and 33% a bachelor's degree or more) and 81.4% of the women had a job. Regarding marital status, 100% of participants lived with their partners, and 59.1% were married. The length of romantic relationships ranged from 1 to 17 years ( M = 6.25, SD = 3.81). Pregnancy was planned in 82.6%.
The regression analysis with socio-demographic characteristics as independent variables and the score of PPD as a dependent variable showed that the model composed by age, length of the romantic relationship, level of education (dummy variable: 1 = high school or university degree; 0 = middle school or elementary school degree), employment status (dummy variable: 1 = employed; 0 = unemployed), and planned pregnancy (dummy variable = 1 = non-planned; 0 = planned) explained only 6% of the variance ( Table 1 ). Specifically, data showed that the severity of PPD was positively affected by the age of women. On the contrary, the length of the relationship with partner, level of education, employment status, and planned pregnancy did not significantly affect the level of PPD.
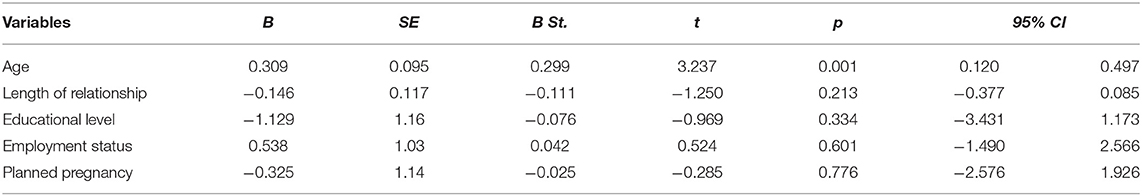
Table 1 . Summary of the linear regression analysis with socio-demographical characteristics as independent variables for PPD score.
Psychopathological Characteristics and PPD Condition
Table 2 shows the means, standard deviations, and pair-wise correlation coefficients for the two dimensions of psychopathological antenatal characteristics (anxiety and depression) and the PPD condition. A high level of PPD was associated with a high level of prenatal anxiety and depression. Moreover, prenatal anxiety and depression were significantly and positively correlated.
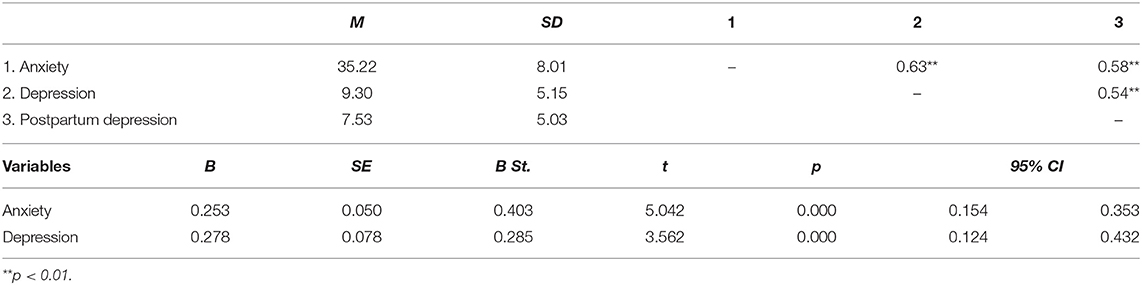
Table 2 . Descriptive statistics, correlations and summary of the linear regression analysis with psychopathological characteristics as independent variables for PPD score.
The linear regression performed with prenatal anxiety and depression on PPD score explained 38% of the variance (see Table 2 ). Both these variables positively affect the level of PPD.
Close Relationships Network and PPD Condition
To obtain a global score of the women's relationship quality with their mothers and fathers, two factor analyses were conducted with the three dimensions of the PBI, for mother and father, separately. Because correlation analyses between the three dimensions of the PBI in relation to the maternal and paternal versions showed that the Overprotection dimension is negatively correlated with Care (maternal: r = −0.77; paternal: r = −0.58) and Encouragement toward autonomy (maternal: r = −0.89; paternal: r = −0.93) dimensions, the Overprotection score was reversed before carrying out the factorial analyses to obtain saturations of the same mark on the hypothetical common factor (the single score of the PBI measure).
The results of the factor analyses showed that the dimensions of the PBI (Care, Encouragement toward autonomy and Low Overprotection) loaded into a single factor for both the maternal and paternal versions. Specifically, regarding the maternal version, the three dimensions accounted for 86.15% of total variance. Regarding the paternal version, the three dimensions accounted for 83.99% of total variance.
In conclusion, both for the mother and father versions, high scores on this dimension express warm, positive and supportive parental behaviors, reflecting a good quality of parental relationships.
In Table 3 , the descriptive statistics of the close relationship variables and their pair-wise correlation coefficients with PPD are shown. The level of PPD was negatively and significantly correlated with the women's relationship quality with their mothers, fathers and romantic partners, and their prenatal attachment to child. Moreover, the prenatal attachment was positively correlated with the quality of the three close relationships (mother, father and partner). Finally, the quality of maternal relationship was significantly and positively correlated with the quality of paternal relationship. Given the high correlation between maternal and paternal relationships ( r = 0.87), in order to avoid multicollinearity problems, a single score of these aspects was calculated. In other words, we composed a score of parental relationship by calculating the mean of the two scores.
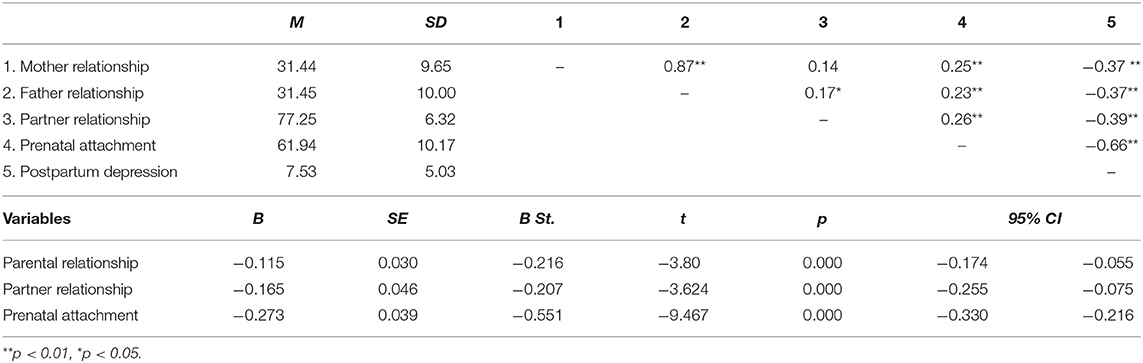
Table 3 . Descriptive statistics, correlations and summary of the linear regression analysis with the quality of parental, romantic and prenatal relationships as independent variables for PPD score.
The linear regression showed that the model composed by parental relationship, romantic relationship and prenatal attachment explained 52% of the variance (see Table 3 ). The quality of parental and romantic relationship and prenatal attachment to child seems to positively affect the level of PPD.
Labor, Delivery, and Birth Outcome Characteristics and PPD Condition
87.6% of the women had spontaneous labor, and in the remaining 12.4% labor was induced. 89.4% of women had vaginal deliveries, and 10.6% had emergency cesarean deliveries. Significant differences emerged with respect to PPD regarding the mode of labor [spontaneous vs. induced: t (159) = −5.311; p = 0.000] and mode [vaginal vs. cesarean: t (159) = 7.429; p = 0.000] of delivery. Specifically, women who had an induced labor showed a higher level of PPD than women who had a spontaneous one. In the same way, women who had a cesarean delivery reported a higher level of PPD than women with vaginal delivery.
Table 4 presents the descriptive statistics and correlation coefficients of all continuous delivery variables.
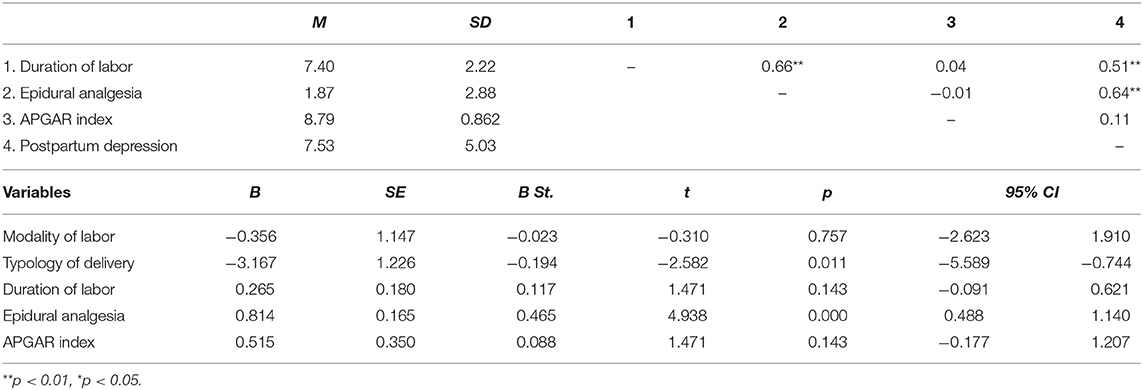
Table 4 . Descriptive statistics, correlations and summary of the linear regression analysis with the delivery characteristics as independent variables for PPD score.
The level of PPD is positively and significantly correlated with the length of labor and the duration of the administration of epidural analgesia. On the contrary, the correlation between PPD and the child's APGAR index is not significant. Finally, the duration of labor is positively and significantly correlated with the duration of the administration of epidural analgesia.
Results of the linear regression showed that the model composed by the variables regarding labor, delivery and birth characteristics explained 44% of the variance (see Table 4 ). Specifically, cesarean delivery (dummy variable: 0 = cesarean delivery; 1 = vaginal delivery), and the duration of the administration of epidural analgesia seem to positively affect the severity of PPD. On the contrary, the results showed the no-significant influences of the modality of labor (dummy variable: 1 = induced labor; 0 = spontaneous labor) and the duration of labor, or the child's APGAR index, in affecting the severity of PPD.
The Stronger Predictors of PPD Condition
Finally, a multiple regression was conducted to explore which of the significant risk factors found in the previously reported analyses make meaningful contributions to the overall prediction of the severity of PPD, which are: age, anxiety, depression, parental relationship, romantic relationship, prenatal attachment, typology of delivery, and epidural analgesia. All these predictors were entered at the first step, using a stepwise method.
Results showed that the model is composed of only four variables, which explain 61% of the PPD total score variance. Specifically, prenatal attachment to child entered into the equation in Step 1, which accounted for the greatest portion of the variance in PPD scores. The duration of the administration of epidural analgesia entered in Step 2, which contributed an additional 10% of variance. The anxiety score entered in Step 3, which contributed an additional 6%. Finally, the quality of romantic relationships entered in Step 4, which contributed an additional 3%. In Table 5 , all statistical results are reported.
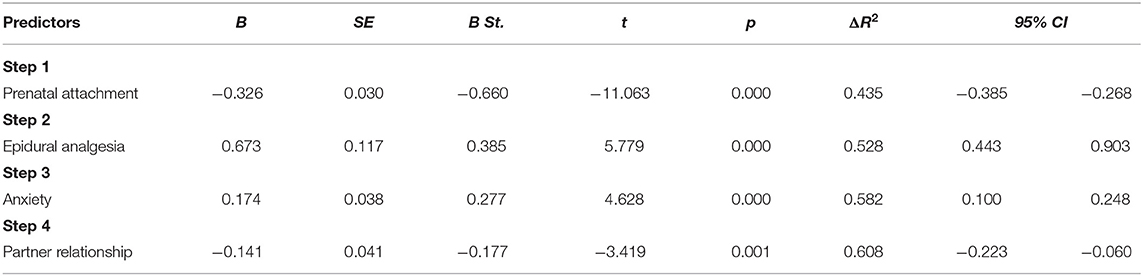
Table 5 . Summary of the linear regression analysis using stepwise method with all risk significant factors as independent variables for PPD score.
Pregnancy and the postpartum period is a delicate moment in a woman's life, characterized by biological, psychological and social change, during which women are at increased risk of emotional vulnerability and depressive symptomatology ( 1 ). This is especially true for nulliparous women, who, in addition to the normal psychic, psychological and relational changes typical of the pregnancy period, are dealing with more specific challenges, such as the transition to motherhood, or the reorganization of mental self-representation. At the first pregnancy, all these changes and reorganizations can represent challenges which are particularly relevant for women, and the presence of problems that prevent them from reaching a good transition to motherhood puts them at greater risk of developing a subsequent depressive symptomology. According to literature, primiparous mothers present an enhanced risk for depression in the postpartum period ( 17 , 18 ) and more severe effects of depression in early interactions with their infants ( 22 ), due to their inexperience compared to multiparous mothers.
In literature, several factors have been found related to PPD, and we believe that the complex interplay of these can be the cause of greater vulnerability in nulliparous women ( 27 – 29 ). For this reason, the main purpose of this study was to explore the role that several sets of variables, such as socio-demographic, individual, relational, and related to delivery characteristics, separately considered, play as risk factors for the onset of postpartum depression in nulliparas. However, to date, no studies have jointly analyzed all these different risk factors. Consequently, the main and second purpose was to verify which have a more significant influence when they are considered together, in order to identify the more important risk factors.
Overall, our results show that, in reference to socio-demographic characteristics, only the age of women was a significant predictor of PPD scores. Older women seem have a higher probability of developing a depressive symptomatology 1 month after childbirth. On the contrary, in line with Roomruangwong's results ( 29 ), we found no significant influences of the level of education, employment status, the length of the romantic relationship, or planned pregnancy.
In reference to psychopathological characteristics, our results showed a strong association between prenatal psychopathology and the possibility to develop PPD. According to previous studies ( 28 , 29 , 53 ), nulliparous with a high level of anxiety and depression during pregnancy tend to develop PPD symptomatology more than women with a low level of these characteristics before delivery. Not surprisingly, due to the high association between antenatal and post-partum depression, the last edition of the DSM ( 9 ) proposed the term “peripartum onset” to indicate the depressive episode occurring during the pregnancy and the first 4 weeks after delivery.
Regarding the relational variables, our results indicated that only the prenatal attachment to child and the quality of romantic relationship affect the level of PPD ( 30 , 32 ). In particular, prenatal attachment, defined as the emotional bond experienced by the parent toward the infant ( 54 ), seems to play a very important role in PPD, given that it involves the maternal disposition toward fetus and a protection attitude toward baby ( 55 , 56 ). New research has suggested that this type of attachment is an indicator of the caregiving system ( 56 , 57 ).
Interestingly, it is not the length of the relationship but its quality that better influences the security and well-being of nulliparous women. In has been widely recognized that the quality of the romantic relationship is a strong protective factor in the life-span ( 58 , 59 ), and this could play an important role, especially in certain periods of life, such as the puerperium ( 60 ). During the transition to parenthood, the couple relationship may be negatively affected during pregnancy, given that birth of the first child leads to partnership re-organization of responsibilities and reciprocal routines, thus decreasing relationship quality ( 61 ). Therefore, a high quality of couple relationship constitutes a protective factor, and a low quality of romantic relationship constitutes a significant risk factor for the development of psychological diseases, such as a higher probability to develop depressive symptoms ( 62 ) and other forms of psychopathology ( 63 ).
The quality of relationship with parents also affects the level of PPD. In reference to a woman's relationship with her parents, this result is convergent with previous studies that have found that the bond quality to mother significantly influences a woman's well-being during pregnancy and after delivery, considerably reducing the risk to develop a PPD condition ( 64 ). Tani et al. ( 65 , 66 ) have shown that the security of attachment to mother affects the quality of prenatal attachment and the consequent ability of the new mother to be sensitive to her newborn's needs, promoting spontaneous caregiving and attachment behavior. Maternal perceived support could also be considered a relevant protector factor: women who reported a high level of maternal social support showed a lower level of PPD symptomatology after labor ( 31 ). However, although in line with previous studies, this study expands on existing literature, showing the protective role of both maternal and paternal relationships on nulliparous women postnatal depression. It is reasonable to suppose that quality of relationship with parents is relevant during the first pregnancy, given that it can help women in the transition to motherhood and the assumption of the maternal role.
Finally, regarding labor factors, our data showed that a longer duration of the administration of epidural analgesia could be considered significant predictors of PPD in nulliparous. As suggested by previous studies, these factors can negatively influence the quality of the birth experience, fostering the possibility of developing a depressive mood, while an easier childbirth experience can act as a protective factor during the vulnerable period after delivery ( 31 , 67 – 69 ). Regarding delivery factors, our findings suggest that emergency cesarean delivery affects post-partum depression in the nulliparous. This seems to confirm that women who express a strong desire to have a natural childbirth during pregnancy, but who must undergo cesarean section, are more prone to risk of postpartum depression ( 70 ).
Finally, our results highlighted no significant influences of the other variables considered, such as the length and the modality of labor and the APGAR index. In our sample, newborns showed good general condition. In fact, only three children (1.9%) obtained a score lower than 7, and no scores lower than six.
The second aim of this study was to explore which, among the above considered risk factors, were the stronger ones. Our analysis showed that, despite the marginal role of variables linked to clinical delivery difficulties, prenatal women's psychopathological characteristics and poor quality of couple relationship, prenatal attachment to child was the most important predictor of PPD, which, by itself, explains almost all the variance of the tested model.
Prenatal attachment expresses the first internalized representation that a pregnant woman develops of her unborn child and the emotional tie with him/her. Therefore, it is reasonable to hypothesize that a nulliparous with a good representation of her future child could experience her pregnancy with positive feelings, and that this, in turn, could improve the transition to her parenting role and well-being.
Extensive literature has shown that women who felt more affection toward their unborn children have more compliance with health practices during pregnancy ( 71 , 72 ), present less clinical complications during delivery, and show less difficulty, more confidence and better adjustment in assuming the new parenting role ( 73 ). Moreover, it has been found that prenatal attachment to the fetus plays a positive and significant role in promoting more adequate mother-child interactions ( 61 ) and spontaneous caregiving and attachment behavior after childbirth ( 65 ). Therefore, it is not surprising that the mother's prenatal attachment to child could represent a key element to improving the health of the mother and child, the outcome being a significant protective factor to prevent PPD onset.
Despite the doubtless interest of these results, there are some limitations to this study. The first is the inclusion criteria. Only nulliparous women with no risk pregnancy, no twins, or previous miscarriage or abortion, were included in this study. Therefore, future research should extend study to samples of women who have twin pregnancies, or with high-risk pregnancies. A second limitation is that our study only investigated the role of relational variables connected to the women's close relationship network, not considering the role that relationships with gynecologists, midwives, and medical and nursing staff play in influencing the mothers' delivery experience during pregnancy and childbirth, and postpartum depression outcomes. An important direction for future research would be to extend this study to other aspects of the women's social network. Providing these additional data could allow us to develop specific and targeted preventive interventions for PPD, and a better understanding of which variables could be important in women with a more complicated history of pregnancy. A third limitation to this study is that PPD was assessed at 1 month post birth. Although it has been recognized that the vulnerability for depression continues for 6 months after delivery ( 14 – 16 ), according to DSM-5, depression with postpartum onset is an episode of major depression that occurs in the 4 weeks following delivery. In any case, further research should extend the follow-up to a longer period of time, for example, 4–6 months of the child's life. It is necessary to underline that the number of comparisons between the methods of birth is very different. In future research, it would be appropriate to have a more homogeneous sample, to compare PPD both after cesarean and after spontaneous or induced vaginal birth.
Finally, further studies with larger samples are desirable to replicate our findings.
Overall, the results of the present study have great relevance for clinical practice. Perinatal depression is an important public health issue with aftermath for mothers, children, and families. This is especially true for women during the first pregnancy, because of their greater emotional vulnerability. Timely screening and appropriate treatment are needed to prevent unnecessary suffering. Until now, screening and preventive health programs have given attention to medical and clinical risk factors. However, our results stress the importance of new focus on more comprehensive care and wellness, suggesting the promotion of mothers' and children's health in perinatal phases by expanding initiatives in clinical practice to additional behavioral and psychosocial screenings. Besides the importance of an early detection of depressive and anxious symptoms in nulliparous women, the present results highlight the relevant role played by relational factors, such as the quality of prenatal attachment to child, the relationship with partner, and the relationship with parents. All these relationships need to be taken into consideration to guarantee a more positive outcome toward the transition to motherhood. Moreover, it may be important to provide more information to women about the various possibilities of labor and delivery: what they are, what consequences they have, not only on the health of the mother and child, but also on the mother-child relationship, in order to allow women to have a more comprehensive understanding of these important aspects.
In conclusion, we believe that these results could have relevant clinical and social implications. Understanding the most important relevant risk factors for PPD is essential for identifying nulliparous pregnant women at risk and promptly intervening with specific preventive health care programs.
Data Availability Statement
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Ethics Statement
The study was conducted in accordance with the guidelines for the ethical treatment of human participants of the Italian Psychological Association. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Ethical Committee of Azienda USL 4 Prato, Italy (no 780/2013).
Author Contributions
MS participated in the development of protocol and analytical framework for the study. Moreover, she contributed to the drafting of the introduction and discussion sections of the manuscript. LP had primary responsibility for protocol development, patient screening, and participant's enrolment. Moreover, she performed the data analysis and contributed to draft the Methods and Materials section. FP revised the manuscript critically for important intellectual content.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Darvill R, Skirton H, Farrand P. Psychological factors that impact on women's experiences of first-time motherhood: a qualitative study of the transition. Midwifery. (2010) 26:3. doi: 10.1016/j.midw.2008.07.006
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Deave T, Johnson D, Ingram J. Transition to parenthood: the needs of parents in pregnancy and early parenthood. BMC Pregnancy Childbirth. (2008) 8:30. doi: 10.1186/1471-2393-8-30
3. Stern DN. The Motherhood Constellation: A Unified View of Parent-infant Psychotherapy . New York, NY: Basic Books (1995).
Google Scholar
4. Slade A, Cohen LJ, Sadler LS, Miller M. The psychology and psychopathology of pregnancy: reorganization and transformation. In: Zeanah CH, editor. Handbook of Infant Mental Health . New York, NY: The Gilford Press (2009). p. 22–39.
5. Cast AD. Well-being and the transition to parenthood: An identity theory approach. Sociol Perspect. (2004) 47:1. doi: 10.1525/sop.2004.47.1.55
CrossRef Full Text | Google Scholar
6. Cox M, Paley B, Burchinal M, Payne C. Marital perceptions and interactions across the transition to parenthood. JMF. (1999) 61:611–25. doi: 10.2307/353564
7. Condon J, Boyce P, Corkindale C. The first time fathers study: a prospective study of the mental health and wellbeing of men during the transition to parenthood. Aust N Z J Psychiatry. (2004) 38:56–64. doi: 10.1111/j.1440-1614.2004.01298.x
8. Banse R. Adult attachment and marital satisfaction: evidence for dyadic configuration effects. JSPR. (2004) 21:273–82. doi: 10.1177/0265407504041388
9. APA (2013). American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed . Arlington, VA: American Psychiatry Publishing. doi: 10.1176/appi.books.9780890425596
PubMed Abstract | CrossRef Full Text
10. Beck C. (1993). Teetering on the edge: a substantive theory of postpartum depression. Nurs Res. 42:42–8. doi: 10.1097/00006199-199301000-00008
11. McCarthy A. Postnatal depression: diagnosis and treatment. Ir Med. (1998) 91:44.
PubMed Abstract | Google Scholar
12. Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:315–23. doi: 10.1192/bjp.bp.116.187179
13. Cox JL, Murray D, Chapman GA. Controlled study of onset, duration and prevalence of postnatal depression. Br J Psychiatry. (1993) 163:27–31. doi: 10.1192/bjp.163.1.27
14. Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. (2001) 323:257–60. doi: 10.1136/bmj.323.7307.257
15. Huang YC, Mathers N. Postnatal depression—Biological or cultural? A comparative study of postnatal women in the UK and Taiwan. J Adv Nurs. (2011) 33:279–87. doi: 10.1046/j.1365-2648.2001.01664.x
16. Vismara L, Rollè L, Agostini F, Sechi C, Fenaroli V, Molgora S, et al. Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: a 3- to 6-months postpartum follow-up study. Front Psychol. (2016) 7:938. doi: 10.3389/fpsyg.2016.00938
17. Satoh A, Kitamiya C, Kudoh H, Watanabe M, Menzawa K, Sasaki H. Factors associated with late post-partum depression in Japan. Jpn J Nurs Sci. (2009) 6:1. doi: 10.1111/j.1742-7924.2009.00121.x
18. Zubaran C, Foresti K. Investigating quality of life and depressive symptoms in the postpartum period. Women Birth. (2011) 24:1. doi: 10.1016/j.wombi.2010.05.002
19. Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: a population-based register study. JAMA. (2006) 296:2582–9. doi: 10.1001/jama.296.21.2582
20. Mancini F, Carlson C, Albers L. Use of the postpartum depression screening scale in a collaborative obstetric practice. JMWH. (2007) 52:429–34. doi: 10.1016/j.jmwh.2007.03.007
21. Glavin K, Smith L, Sørum R. Prevalence of postpartum depression in two municipalities in Norway. Scand J Caring Sci. (2009) 23:705–10. doi: 10.1111/j.1471-6712.2008.00667.x
22. Righetti-Veltema M, Conne-Perréard E, Bousquet A, Manzano J. Postpartum depression and mother-infant relationship at 3 months old. J Affect Disord. (2002) 70:291–306. doi: 10.1016/S0165-0327(01)00367-6
23. Van den Bergh BRH, Mulder EJH, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. (2005) 29:237–58. doi: 10.1016/j.neubiorev.2004.10.007
24. Henderson JJ, Evans SF, Straton JA, Priest SR, Hagan R. Impact of postnatal depression on breastfeeding duration. Birth. (2003) 30:175–80. doi: 10.1046/j.1523-536X.2003.00242.x
25. Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: a sensitive period? J Am Acad Child Adolesc Psychiatry. (2010) 49:7. doi: 10.1016/j.jaac.2010.03.012
26. Glasheen C, Richardson GA, Fabio A. (2010). A systematic review of the effects of postnatal maternal anxiety on children. Arch Womens Ment Health. (2010) 13:1. doi: 10.1007/s00737-009-0109-y
27. Ross LE, Sellers EM, Gilbert Evan SE, Romach MK. Mood changes during pregnancy and the postpartum period: development of a biopsychosocial model. Acta Psychiatr Scand. (2004) 109:457–66. doi: 10.1111/j.1600-0047.2004.00296.x
28. Coelho HF, Murray L, Royal-Lawson M, Cooper PJ. Antenatal anxiety disorder as a predictor of postnatal depression: a longitudinal study. J Affect Disord. (2011) 129:1–3. doi: 10.1016/j.jad.2010.08.002
29. Roomruangwong C, Withayavanitchai S, Maes M. (2016). Antenatal and postnatal risk factors of postpartum depression symptoms in Thai women: a case-control study. Sex Reprod Healthc. (2016) 10:25–31. doi: 10.1016/j.srhc.2016.03.001
30. Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan PH, et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med. (2000) 30:1273–81. doi: 10.1017/S0033291799002937
31. Tani F, Castagna V. Maternal social support, quality of birth experience, and post-partum depression in primiparous women. J Matern Fetal Neonatal Med. (2016) 30:6. doi: 10.1080/14767058.2016.1182980
32. Sapkota S, Kobayashi T, Takase M. Husbands' experiences of supporting their wives during childbirth in Nepal. Midwifery. (2012) 28:1. doi: 10.1016/j.midw.2010.10.010
33. Priel B, Besser A. Vulnerability to postpartum depressive symptomatology: dependency, self-criticism and the moderating role of antenatal attachment. J Soc Clin Psychol. (1999) 18:2. doi: 10.1521/jscp.1999.18.2.240
34. Brealey SD, Hewitt C, Green JM, Morrell J, Gilbody S. Screening for postnatal depression: is it acceptable to women and healthcare professionals? A systematic review and meta-synthesis. J Reprod Infant Psychol. (2010) 28:4. doi: 10.1080/02646838.2010.513045
35. Mustaffa MS, Marappan D, Abu MS, Khan A, Ahmad R. Social support during prenatal and postnatal stage: influence on maternal depression and mental well-being. Procedia Soc Behav Sci. (2014) 143:417–22. doi: 10.1016/j.sbspro.2014.07.506
36. Scope A, Booth A, Morrell CJ, Sutcliffe P, Cantrell A. Perceptions and experiences of interventions to prevent postnatal depression. A systematic review and qualitative evidence synthesis. J Affect Disord. (2017) 210:1. doi: 10.1016/j.jad.2016.12.017
37. McCoy SJB, Beal JM, Shipman SBM, Payton ME, Watson GH. (2006). Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. J Am Osteopath Assoc. (2006) 106:193–8.
38. Porter CL, Hsu HC. First-time mothers' perceptions of efficacy during the transition to motherhood: links to infant temperament. J Fam Psychol. (2003) 17:1. doi: 10.1037//0893-3200.17.1.54
39. Davis L, Edwards H, Mohay H, Wollin J. The impact of very premature birth on the psychological health of mothers. Early Hum Dev. (2003) 73:61–70. doi: 10.1016/S0378-3782(03)00073-2
40. Rubertsson C, Waldenstrom U., Wickberg B. (2003). Depressive mood in early pregnancy: prevalence and women at risk in a national Swedish sample. J Reprod Infant Psychol. 21:2. doi: 10.1080/0264683031000124073
41. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. (1983). State-Trait Anxiety Inventory for Adults: Manual, Instrument and Scoring Guide . Mind Garden: Consulting Psychologists Press (1983). doi: 10.1037/t06496-000
CrossRef Full Text
42. Predabissi L, Santinello M. Edizione Italiana STAI . Firenze: Giunti OS (1989).
43. Chinchilla-Ochoa D, Barriguete-Chávez Peón P, Farfán-Labonne BE, Garza-Morales S, Leff-Gelman P, Flores-Ramos M. Depressive symptoms in pregnant women with high trait and state anxiety during pregnancy and postpartum. Int J Womens Health. (2019) 11:257–65. doi: 10.2147/IJWH.S194021
44. Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression . New York, NY: Guilford Press (1979).
45. Ghisi M, Flebus GB, Montano A, Sanavio E, Sica C. Beck Depression Inventory, 2nd ed . Firenze: Organizzazioni Speciali (2006).
46. Parker G, Tupling H, Brown LB. A parental bonding instrument. Br J Med Psychol. (1979) 52:1. doi: 10.1111/j.2044-8341.1979.tb02487.x
47. Bonaiuto M, Perucchini P, Pierro A. L'adolescente e i membri significativi della sua rete sociale [Adolescent and significant members of his social network]. Età Evol. (1997) 57:40–56.
48. Ponti L, Guarnieri S, Smorti A, Tani F. A measure for the study of friendship and romantic relationship quality from adolescence to early-adulthood. TOPSY J. (2010) 12:3. doi: 10.2174/1874350101003010076
49. Müller ME. Development of the prenatal attachment inventory. West J Nurs Res. (1993) 15:2. doi: 10.1177/019394599301500205
50. Della Vedova AM, Dabrassi F, Imbasciati A. (2008). Assessing prenatal attachment in an Italian women sample. J Reprod Infant Psychol. (2008) 26:86–98. doi: 10.1080/02646830701805349
51. Benvenuti P, Ferrara M, Niccolai C, Valoriani V, Cox JL. The Edimburgh Postnatal Depression Scale: validation for an Italian sample. J Affect Disord. (1999) 53:2. doi: 10.1037/t11281-000
52. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
53. Norhayati MN, Hazlina NH, Asrenee AR, Emilin WM. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. (2015) 175:1. doi: 10.1016/j.jad.2014.12.041
54. Condon JT, Corkindale CJ. The assessment of parent-to-infant attachment: development of a self-report questionnaire instrument. J Reprod Infant Psychol. (1998) 16:1. doi: 10.1080/02646839808404558
55. Condon JT. The assessment of antenatal emotional attachment: development of a questionnaire instrument. Br J Med Psychol. (1993) 66:2. doi: 10.1111/j.2044-8341.1993.tb01739.x
56. Walsh J, Hepper EG, Marshall BJ. Investigating attachment, caregiving, and mental health: a model of maternal-fetal relationships. BMC Pregnancy Childbirth. (2014) 14:383. doi: 10.1186/s12884-014-0383-1
57. Brandon AR, Pitts S, Denton WH, Stringer CA, Evans HM. A history of the theory of prenatal attachment. J Prenat Perinat Psychol Health. (2009) 23:201–22.
58. Diener M, Diener McGravan MB. What makes people happy? A developmental approach to the literature on family relationships and well-being. In: Eid M, Larsen RJ, editor. The Science of Subjective Well-being . New York, NY: Guilford (2008). p. 347–75.
59. Guarnieri S, Smorti M, Tani F. Attachment relationships and life satisfaction during emerging adulthood. Soc Indic Res. (2015) 121:3. doi: 10.1007/s11205-014-0655-1
60. Yusuff ASM, Tang L, Binns CW, Lee AH. Prevalence and risk factors for postnatal depression in Sabah, Malaysia: a cohort study. Women Birth. (2015) 28:1. doi: 10.1016/j.wombi.2014.11.002
61. Mazzeschi C, Pazzagli C, Radi G, Raspa V, Buratta L. Antecedents of maternal parenting stress: the role of attachment style, prenatal attachment, and dyadic adjustment in first-time mothers. Front Psychol. (2015) 6:1443. doi: 10.3389/fpsyg.2015.01443
62. Beach SH, Katz J, Kim S, Brody GH. Prospective effects of marital satisfaction on depressive symptoms in established marriages: a dyadic model. J Soc Pers Relat. (2003) 20:6. doi: 10.1177/0265407503020003005
63. South SC, Krueger RF. Understanding general and specific connections between psychopathology and marital distress: a model based approach. J Abnorm Psychol. (2011) 120:4. doi: 10.1037/a0025417
64. McMahon CA, Barnett B, Kowalenko NM, Tennant CC. Maternal attachment state of mind moderates the impact of postnatal depression on infant attachment. J Child Psychol Psychiatry (2006) 47:660–9. doi: 10.1111/j.1469-7610.2005.01547.x
65. Tani F, Castagna V, Ponti L. Women who had positive relationships with their own mothers reported good attachments to their first child before and after birth. Acta Paediatr. (2017) 107:4. doi: 10.1111/apa.14162
66. Tani F, Castagna V, Ponti L. Mothers' social perceived support, anxiety and prenatal attachment to child: which direct and indirect influences on delivery clinical indices? Int J Health Sci Res. (2017) 7:346–52.
67. Blom EA, Jansen PW, Verhulst FC, Hofman A, Raat H, Jaddoe VWV, et al. Perinatal complications increase the risk of postpartum depression. The Generation R Study. BJOG. (2010) 117:11. doi: 10.1111/j.1471-0528.2010.02660.x
68. Smorti M, Ponti L, Tani F. Maternal depressive symptomatology during pregnancy is relevant risk factor affecting newborn's health: a longitudinal study. J Reprod Infant Psychol. (2019) 39:492–7. doi: 10.1080/02646838.2019.1581919
69. Smorti M, Ponti L, Tani F. The effect of maternal depression and anxiety on labour and the well-bing of the newborn. J Obstet Gynaecol. (2019) 39:492–7. doi: 10.1080/01443615.2018.1536697
70. Houston KA, Kaimal AJ, Nakagawa S, Gregorich SE, Yee LM, Kuppermann M. Mode of delivery and postpartum depression: the role of patient preferences. Am J Obstet Gynecol. (2015) 212:2. doi: 10.1016/j.ajog.2014.09.002
71. Alhusen JL, Gross D, Hayat MJ, Rose L, Sharps P. The role of mental health on maternal-fetal attachment in low-income women. J Obstet Gynecol Neonatal Nurs. (2012) 41:6. doi: 10.1111/j.1552-6909.2012.01385.x
72. Sadat Maddahi M, Dolatian M, Khoramabadi M, Talebi A. Correlation of maternal-fetal attachment and health practiced during pregnancy with neonatal outcomes. Elecron Psys. (2016) 8:7. doi: 10.19082/2639
73. Shah PE, Fonagy P, Strathearn L. Is attachment transmitted across generations? The plot thickens. Clin Child Psychol Psychiatry. (2010) 15:3. doi: 10.1177/1359104510365449
Keywords: postnatal depression, childbirth, maternal mental health, risk factor, nulliparous women
Citation: Smorti M, Ponti L and Pancetti F (2019) A Comprehensive Analysis of Post-partum Depression Risk Factors: The Role of Socio-Demographic, Individual, Relational, and Delivery Characteristics. Front. Public Health 7:295. doi: 10.3389/fpubh.2019.00295
Received: 03 April 2019; Accepted: 01 October 2019; Published: 24 October 2019.
Reviewed by:
Copyright © 2019 Smorti, Ponti and Pancetti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martina Smorti, martina.smorti@unipi.it ; Lucia Ponti, pontilucia@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

The Debate about Causes of Postpartum Depression
Why some women struggle emotionally after childbirth.
Posted March 31, 2013
- What Is Depression?
- Take our Depression Test
- Find a therapist to overcome depression
(Written on the last day of Women's History Month)
Pregnancy is in the news with the announcement that Kate Middleton is expecting a baby and that maybe she even let it slip that its sex is female.
Pregnant women and new mothers are supposed to feel happy, since after all, this is what we women are allegedly born to do: Give birth and nurture.
But also in the news are some recent studies of postpartum depression , the very term telling us that it's not all sunshine and smiles.
About 35 years ago, when I started thinking about what became Don't Blame Mother: Mending the Mother-Daughter Relationship (first worked on it in the late 1970s, first edition published 1989, THE NEW Don't Blame Mother published in 2000)*, I was troubled that the talk about postpartum depression always seemed based on the notion that women's hormones somehow made them "go crazy" after they gave birth. Why did that trouble me? Because I had myself been through the fears and anxieties that so many women go through during pregnancy -- Will the baby be healthy? How in the world will I know how to be a good mother? How can I protect the baby and growing child from the physical dangers and the many heartaches the world can bring? -- and the huge sense of responsibility of being a new mother, when we realize that being female does not automatically give us all the answers about how to be a good mother.
Consciously or not, both women and men in this country and many others know that if anything goes wrong with one's baby, child, teenager , or even adult offspring, the mother will almost invariably be blamed, whether or not she is at fault. In fact, after I raised concern about mother-blame at the clinic where I was working and was told my the psychiatrist who was my team leader that he thought I was just imagining how common it was, and that that was because I was a woman, a mother, and -- horrors! -- a feminist, I decided to put my training as a researcher to use, to see if he was right. With Ian Hall-McCorquodale, I did a systematic study of mother-blame in major clinical journals and found that it was even more rampant, unwarranted, and horrific than I had feared.** Despite the glorious aspects of having a child, it is damned hard to know every moment that you will be blamed for virtually every problem the child might have, and that anxiety -- no, more appropriate to call it fear , even terror, because nothing less than your child's welfare is at stake -- plagues so many mothers. In fact, just a few days ago, I was a guest on a radio show on which another guest said repeatedly that if anything goes wrong, it is right to blame the mother, because her relationship to the child is closer than that of anyone else. Whether or not you believe that her statement about closeness is true -- and it certainly is not true of some mothers, and of course some fathers are as close to or even closer to their children than are the children's mothers -- there simply is no epidemic of father-blame that remotely approaches the pervasiveness of mother-blame.
Mothers, as I wrote in 1989/2000, raise their children in a world permeated by motherhood myths, some of which set standards so high that no human could reach them (mothers are 100% nurturant 100% of the time, good mothers never get angry, mothers instinctively know everything they need to know about raising healthy children) and some of which urge us to take even good things that mothers do (e.g., being close, loving, and caring) and transform them into "proof" that mothers are bad (e.g., mothers' closeness is smothering).
There is in addition the terrible isolation that many mothers feel. The isolation stems partly from demographic changes in recent decades, leading to the geographic isolation of mothers from family members and/or frequent moves to new communities in search of employment, leading to geographic distance from close friends. The isolation also stems from the pressure on women to be happy and serene as mothers, even as brand-new mothers whose bodies may be physically depleted from pregnancy and/or labor and delivery. In fact, it struck me in the late 1970s how positively absurd it is to expect that the very person whose body has just been through the physical demands of pregnancy, labor, and delivery is the one person who is expected to be ready, able, and delighted to do the lion's share of caring for the newborn. If someone told us that a neurosurgeon who had just been on her feet doing brain surgery for 72 hours straight was about to operate on someone we love, we'd ask for a better-rested surgeon.
Still another cause of social isolation is this: Given that a new mother is supposed to feel simply elated, fully competent, and even calm, many women are mortified when they feel terrified, clueless, and exhausted, and the last thing they need is for anyone to find out about these "inappropriate, unmotherly" feelings. They assume something is wrong with them for not simply having the emotions depicted on greeting cards about new babies.
When I think about my own experience, I know -- have always known -- how privileged I was as a new mother, because despite all of the concerns, fears, and insecurity I felt, I did not at the time have to worry about whether I would have enough money to support a child. And as a white woman, I was not subjected to racism . I was not a battered wife. If any of that had been different, how much more reason would I have had for anxiety and despair.
Should we surprised, then, by a recent report*** that at one obstetrical hospital, 14% of the women "screened positive for depression"? In fact, I am surprised that that percentage is not higher. But let's look further at that report. Rather than being a study of the kinds of factors described above and how they affect new mothers, this one was designed as a " psychiatric " investigation: Their orientation was to call upset in new mothers psychiatric disorder instead of understandable responses to the intense pressures and isolation of these women. It's a simple matter to classify their fear, insecurity, and even despair of being able to measure up to the impossible motherhood standards as psychiatric disorder. In fact, that is literally all it takes: Note these feelings, and label them mental illness, which is how "postpartum depression" is often classified. Then the new mother has an additional burden: Her totally understandable feelings have been classified as sickness, and she feels even more than before that she is defective, that the fault is simply her own. She becomes alarmed that her alleged mental illness is now something else that will put her baby at risk. And too often, another consequence of labeling postpartum upset and suffering as mental illness is that the woman is put on psychiatric drugs that, as always with such drugs, can sometimes help some people, at least for awhile and maybe for longer, but on balance do more harm than good.**** Furthermore, in new mothers, taking psychiatric drugs can seriously harm the baby through breastfeeding, which therefore must be stopped.
It is alarming that calling postpartum depression a mental illness takes the focus off the many social changes we need to make to reduce the burdens on new mothers, such as providing more social support and practical help, providing better healthcare for mother and baby, and working hard to expose the myths about motherhood and reduce the mother-blame that put unnecessary and enormous burdens on mothers.

Another new study scheduled for future publication***** reveals that -- surprise, surprise! -- when new mothers feel that they have more social support from their families, the rate of postpartum depression declines. They say that this is the case for women from "diverse socioeconomic and ethnic/racial backgrounds." The authors of this study also report that that social support dampened the mother's "corticotropin-releasing hormone" during pregnancy and that that helped reduce postpartum upset. It is important to know that that hormone is a response to what is euphemistically and vaguely called " stress " but that I prefer to call intense emotional and social pressures. Unlike the unfounded claims that what gets called "mental illness" is caused not by what happens to people in their lives but rather by abnormal neurochemistry or "broken brains," there is now this proof the cause-effect relationship is the reverse: Lack of social support causes a physiological change, and it is known that problems with stress hormones can cause or intensify exhaustion, the last thing that a new mother needs. So in the absence of adequate social support, it makes sense that the rise in this hormone intensifies the new mother's exhaustion, which understandably increases the chances that she will feel despair about the prospect of being able to provide adequate care for her newborn. All the more reason to provide more support of various kinds for new mothers, rather than assuming they have mental disorders and moving immediately to drug them. And as shown in this new study, the earlier that that support is provided, the more effective it is in reducing problems for the mothers.
One final thought is about that word "depression." The brilliant David Jacobs and David Cohen challenge us to think about how freely, vaguely, and variously it is used.****** Their argument about its lack of specificity is so compelling that it has made me realize that when someone tells me they are "depressed," I know little other than that they are feeling badly somehow. I have adopted the practice of asking people who use that word to answer the following question: "If you were not going to use the word 'depressed,' what word or words would describe what you feel?" And I have been amazed by how much more clearly the person is able to specify what they feel and how much easier it is for me to understand -- and relate to -- what they then say. Usually, their response includes one or more of the following: sad, grief -stricken, lonely, helpless, hopeless, wistful, nostalgic, longing, or despondent. I conclude this essay by suggesting that for women experiencing postpartum emotional problems (as for anyone else who is suffering emotionally), we try to help them understand more specifically what they are feeling, because if they come up with any of the words in the list above, it is easier both for them and for us to know what might help.
*Caplan, Paula J. The New Don’t Blame Mother: Mending the Mother-Daughter Relationship. New York: Routledge, 2000. **Caplan, Paula J., & Hall-McCorquodale, Ian. Mother-blaming in major clinical journals. American Journal of Orthopsychiatry, 55, 1985, 345‑353; and Caplan, Paula J. & Hall-McCorquodale, Ian. The scapegoating of mothers: A call for change. American Journal of Orthopsychiatry, 55, 1985, 610‑613. ***Postpartum Depression: Surprising Rate of Women Depressed After Baby. 2013, March 13. http://www.sciencedaily.com/releases/2013/03/130314124618.htm ****Whitaker, Robert. Anatomy of an Epidemic. 2010. *****Hahn-Holbrook, Jennifer; Dunkel Schetter, Christine; Arora, Chander; & Hobel, Calvin J. Placental corticotropin-releasing hormone mediates the association between prenatal social support and postpartum depression. Clinical Psychological Science. 2013. ******Jacobs, D. H., and Cohen, D. (2010). The make-believe world of antidepressant randomized controlled trials---An afterword to Cohen and Jacobs (2010). The Journal of Mind and Behavior 31, 25-36.
©Copyright 2013 by Paula J. Caplan All rights reserved

Paula J. Caplan, Ph.D. , a clinical and research psychologist, is an associate at Harvard University's DuBois Institute and former fellow in Harvard Kennedy School's Women and Public Policy Program.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Womens Health
Treatment of postpartum depression: clinical, psychological and pharmacological options
Elizabeth fitelson.
4 PGY-I Resident in Psychiatry, Department of Psychiatry, Columbia University Medical Center, New York, NY, USA
Allison Scott Baker
3 Child and Adolescent Psychiatry Fellow, Division of Child Psychiatry
Kristin Leight
2 Attending Psychiatrist, TheWomen’s Program
Postpartum depression (PPD) is a common complication of childbearing, and has increasingly been identified as a major public health problem. Untreated maternal depression has multiple potential negative effects on maternal-infant attachment and child development. Screening for depression in the perinatal period is feasible in multiple primary care or obstetric settings, and can help identify depressed mothers earlier. However, there are multiple barriers to appropriate treatment, including concerns about medication effects in breastfeeding infants. This article reviews the literature and recommendations for the treatment of postpartum depression, with a focus on the range of pharmacological, psychotherapeutic, and other nonpharmacologic interventions.
Introduction
Epidemiology of postpartum depression.
Estimates of prevalence of PPD in the US, UK and Australia range from 7%–20%, with most studies suggesting rates between 10%–15%. 6 , 7 Significant risk factors for PPD include a history of depression prior to or during pregnancy, anxiety during pregnancy, experiencing stressful life events during pregnancy or the early puerperium, low levels of social support 8 or partner support, 9 low socioeconomic status, and obstetric complications. 7 Although mental health often is not prioritized as a problem in poorer countries where access to basic nutrition and health care are not consistent, the evidence suggests that postnatal depression may be both more common and more grave for women and their children in low-income countries. The limited data from resource-constrained countries suggests that rates of depression in mothers of young infants exceeds 25%, 10 and in some settings may be as high as 60%. 11 The intersection of cultural, interpersonal and socioeconomic factors may also confer significant risk of PPD: in one study in Goa, India, risk for depression after delivery increased with economic deprivation, marital violence, and female gender of the infant. 12
Negative effects of maternal depression
Untreated maternal depression is associated with serious morbidity for the mother, the infant, and the family system. Perinatal depression causes significant suffering in women at a time when personal or societal notions of motherhood as a uniquely joyful, if tiring, experience may be incongruous with the depressed woman’s ability to feel gratification in the mothering role, 13 connect with her infant, or carry out the often overwhelming tasks of caring for a new baby. 14 Such a disconnect can reinforce the disabling sense of isolation, guilt, helplessness and hopelessness that frequently characterize the depressed state. Women with PPD are at higher risk for smoking, 15 alcohol or illicit substance abuse, 16 and are more likely than nondepressed mothers to experience current or recent physical, emotional, or sexual abuse. Although rates of suicide for women during pregnancy and the puerperum are lower than the general population, suicide is an important cause of maternal mortality. 17 Self-inflicted injury is the leading cause of one-year maternal mortality in the United Kingdom. 18 A recent World Health Organization report on women’s health identifies self-inflicted injury as the second leading cause of maternal mortality in high-income countries; suicide remains an important cause of maternal deaths in moderate and low-income countries. 19 Intrusive thoughts of accidental or intentional harm to the baby are common in the early postpartum time. 20 These thoughts are more frequent and distressing in women with postpartum depression; 21 however, nonpsychotic depressed women are unlikely to commit infanticide. 22
The adverse impact of maternal depression on infant outcomes has also been studied. Depression has significant negative effects on a mother’s ability to interact appropriately with her child. 13 Depressed women have been found to have poorer responsiveness to infant cues 23 and more negative, hostile or disengaged parenting behaviors. 24 These disruptions in maternal-infant interactions have been associated with lower cognitive functioning and adverse emotional development in children, and they appear to be universal across cultural and economic divides. 25 , 26 Other parenting behaviors are also affected, including problematic sleep habits, lower preventative health care utilization and undesirable safety practices. 26 Chronic depression in mothers places children at higher risk for behavioral problems 27 and later psychopathology, including anxiety, disruptive, and affective disorders; conversely, remission of depression in mothers is associated with reduction or remission in the children’s psychiatric diagnoses. 28 Maternal depression also increases the risk for negative infant feeding outcomes, including lower rates of initiating or maintaining breastfeeding, lower levels of breastfeeding self-efficacy, and more difficulties while breastfeeding. 29 In low-income countries, maternal depression has been associated with both malnutrition and higher rates of diarrheal illness in children. 30
Diagnosis of postpartum depression
The diagnostic criteria for a Major Depressive Episode (MDE) as defined by the Diagnostic and Statistical Manual (DSM-IV) do not differ in the postpartum period as compared to other times, and include at least 2 weeks of persistent low mood or anhedonia, as well as at least four of the following: increased or decreased appetite, sleep disturbance, psychomotor agitation or retardation, low energy, feelings of worthlessness, low concentration, and suicidal ideation. 31 A MDE may be classified as having a postpartum onset if the depressive symptoms begin within the first 4 weeks after delivery. However, studies suggest that depressive episodes are significantly more common in women in the first three months after delivery, 32 and an increased vulnerability to psychiatric illness may persist for a year or more. 33 It is important to differentiate PPD from other psychiatric and nonpsychiatric diagnoses. The “postpartum blues” or “baby blues” is a transient mood disturbance that affects up to 75% of new mothers in the 10 days following delivery, and consists of crying, irritability, fatigue, anxiety, and emotional lability. Symptoms are generally mild and self-limited, and do not involve total loss of pleasure or interest, persistent low mood, or suicidal ideation. 34 On the other extreme, postpartum psychosis is a psychiatric emergency that requires immediate intervention, and is characterized by the rapid onset of severe mood swings, a waxing and waning sensorium, delusions, hallucinations or disorganized behaviors, and a relatively high incidence of suicidal ideation or homicidal ideation toward the infant. 35 Women presenting with a depressive episode, mood elevation, or psychotic symptoms should be screened for any prior history of mania or hypomania to rule out previously undiagnosed bipolar disorder. 36 Anxiety disorders are common in perinatal women, and women may have depression comorbid with obsessive-compulsive symptoms, generalized anxiety disorder, panic disorder or post-traumatic stress disorder. 37 Substance use and medical causes of psychiatric symptoms, such as thyroid disorders, should also be considered.
Screening for postpartum depression
To try to mitigate these serious adverse outcomes of PPD, there has been increasing focus on the importance of early and accurate detection and treatment of depression after or during pregnancy. 38 Identification of depression in the postpartum period may be complicated by some of the normal physical and emotional demands of new motherhood, including changes in energy and appetite, sleep deprivation, and heightened concern for the infant. Experts have recommended screening for PPD at the first postnatal obstetrical visit (usually 4–6 weeks after delivery), 39 or in the family practice 40 or pediatric setting, 41 as these are the most widespread points of interaction with the health care system for new mothers within the first three months of delivery. The most commonly used screening tool for PPD is the Edinburgh Postnatal Depression Scale (EPDS), 42 a 10-item self-report that emphasizes emotional and functional factors rather than somatic symptoms. Although variability in sensitivity and specificity occurs across languages and cultures, 11 , 43 a reasonable cutoff for a positive screen on the EPDS is ≥13 (out of a possible 30), though special note should be made of any positive responses to Item 10 assessing suicidal ideation. 39 , 43 Other commonly used screening tools with evidence of validity in the puerperium include the Postpartum Depression Screening Scale (PDSS), 44 as well as the 9-item Physician’s Health Questionnaire (PHQ-9). 45 It should be emphasized that these instruments are screening tools which will generate a certain number of false-positives; diagnosis of depression must be confirmed by clinical interview.
Discusssion
Pharmacological treatments for postpartum depression, antidepressant medication.
A small but growing literature suggests that postpartum depression can be thought of as a variant of major depression that responds similarly to antidepressant medication. 46 , 47 Concerns unique to pharmacologic treatment of PPD include metabolic changes in the postpartum period, exposure of the infant to medication in breast milk, the effect of depression and treatment on the ability of the depressed mother to care for a new baby, and the perceived stigma of being seen as a “bad mother” for requiring medication. 48 – 50 These factors, as well as the woman’s level of distress, access to care, and experience with past treatment may influence the decision of the patient and her caregiver regarding the choice of pharmacologic and nonpharmacologic treatments for PPD. Data comparing the effectiveness of medication against other treatment modalities for PPD are scarce, though do suggest that medications are at least as effective as most psychological interventions based on effect size. 51 To date, four randomized controlled studies on the treatment of PPD with antidepressant medications have been published, along with several open trials. Additionally, two randomized studies have looked at the prevention of PPD with antidepressant medication.
In a study of 87 women with major or minor depression in the postpartum period, subjects were randomized to one of four groups receiving either fluoxetine or placebo plus one or six cognitive behavioral therapy (CBT) based counseling sessions. 52 Breastfeeding mothers were excluded from the study. Improvement was seen in all groups, with greater reduction in depression severity in the fluoxetine group compared to the placebo medication, and greater improvement with six counseling sessions compared to one session. Women receiving both fluoxetine and counseling did not differ significantly in outcome compared to women who received fluoxetine alone. Because the mean baseline level of depressive symptoms based on rating scales was mild, the findings are not easily generalized to a population with more severe postpartum depression.
A subsequent study randomized 35 women with postpartum depression and comorbid anxiety to receive paroxetine or paroxetine plus CBT for 12 weeks. 53 Both groups showed significant improvement in depressive and anxiety symptoms (response rates 87.5% in the paroxetine group and 78.9% in the combined group) without significant differences between groups. The study did not include a placebo arm, making analysis of the specific effects of either intervention difficult. A third study compared paroxetine to placebo in an 8-week randomized controlled trial. 54 The attrition rate in this study was high, with only 31 of 70 participants completing the study (17 in the paroxetine arm and 14 in the placebo arm), but the authors found lower mean severity scores and a higher remission rate after 8 weeks of treatment with paroxetine compared to placebo.
Very few studies have compared different classes of medications used in postpartum depression. One comparative study found treatment with nortriptyline to yield similar outcomes as treatment with sertraline. 55 After 8 weeks of treatment in this large, randomized, double-blind trial, both groups showed improvement, and response rates (nortriptyline 69%, sertraline 56%), remission rates (nortriptyline 48%, sertraline 46%) and side effect burden were similar between groups at week 4, 8 and 24, though side effect profiles differed. There was no placebo arm. The response rate could be predicted earlier in the group receiving sertraline, but the overall response rates were equivalent. Sub-analyses of this study revealed an improvement in maternal role function 56 and sexual function 57 that was equivalent in both groups.
Several open studies have found sertraline, 58 venlafaxine, 59 nefazodone, 60 fluvoxamine, 61 and bupropion 62 to be effective in the treatment of postpartum depression. These studies have been small, with 4–15 participants, lacked control groups, and in several cases were sponsored by the pharmaceutical companies manufacturing the studied drug. Though there is little data comparing medications to placebo in the perinatal population, taken together, data from both the controlled and open studies suggest that antidepressants typically used to treat major depression are equally effective in postpartum depression, without clear differences between medications in efficacy and side effect burden. Therefore, some experts recommend that if a patient has responded to a specific antidepressant in the past, that medication should be among the first to be considered in treating her depression in the postpartum. 63
Two placebo-controlled studies have looked at the role of medication in preventing recurrent PPD. In one small randomized placebo controlled pilot study, sertraline initiated shortly after birth for nondepressed women with at least one prior episode of PPD was found to prevent recurrence and prolong time to relapse. 64 However, in another study, no difference was found in rates of recurrence or time to relapse between patients receiving nortriptyline and patients receiving placebo: one out of four women in both groups suffered a relapse within the 20-week study period. 65 Further research is needed to conclude whether initiation of antidepressants after childbirth in a select group of high risk women is preventative against postpartum depression.
Breastfeeding considerations
The benefits of breastfeeding have been well described 66 – 73 and have led the World Health Organization, the American Academy of Pediatrics and the American Academy of Family Practitioners to recommend breastfeeding for at least the first 6 months for most women. 66 , 67 , 73 Potential effects of antidepressant medication on breastfeeding are of concern to many mothers and clinicians. 49 , 74 Neonates and young infants are especially vulnerable to potential drug effects due to their immature hepatic and renal systems, immature blood–brain barriers, and developing neurological systems. 75 , 76 Because relatively little is known about the effects of antidepressant medication in breast milk, some experts have recommended nonpharmacologic treatment modalities when possible, particularly for mild to moderate depression. 76 However, non-pharmacologic treatments are not effective for some women, and may not be accessible for many women.
Information about the effects on infants of exposure to anti-depressants through breast milk is limited to case reports and small studies, with little prospective data. 77 , 78 Several reviews of the pooled available data on antidepressant medication and breastfeeding have concluded that among the serotonergic reuptake inhibitors (SSRIs), sertraline and paroxetine are least likely to be detectable in infant plasma, and have been associated with rare, if any, adverse events in infants, whereas fluoxetine and citalopram appear to have higher passage through breast milk. 75 , 79 – 81 Individual cases of suspected adverse effects that have been reported in infants of breastfeeding mothers on antidepressant medications have ranged from mild to more serious, and include sleep changes, gastrointestinal problems, respiratory problems, and seizure. In most cases, reported effects have been mild and resolved with cessation of the medication or breastfeeding. These adverse events have been reported in the context of mothers taking citalopram, escitalopram, fluoxetine, doxepin and bupropion, 79 – 81 though rates and causality are difficult to assess from case reports, and other studies have reported no adverse effects with the same medications. Given the lower infant blood levels and fewer adverse reports, paroxetine or sertraline may be the most prudent choice for a patient who is naïve to antidepressant medication prior to the postpartum episode. However, adverse events have not been definitively linked to elevated plasma levels in infants; conversely, there is little data to suggest that undetectable levels of antidepressant medication ensure infant safety in the long term. In an effort to determine whether even low-level SSRI exposure through breast milk has central effects in infants, Epperson and colleagues found in separate studies that while sertraline and fluoxetine had the expected significant effects on the platelet 5-HT transporter of mothers taking the medication, their breastfed infants did not experience a significant change in 5-HT platelet transporters. 82 , 83 Whether the lack of effect on peripheral transporters can be extrapolated to predict no effects in the central nervous system of infants remains unclear, though the results are encouraging. Among tricyclic antidepressants, nortriptyline has the most data supporting safety during breastfeeding, whereas doxepin is considered relatively contraindicated. 80 , 82 Information on the newer antidepressant medications is sparse, but few adverse effects have been reported. 80
The long-term risks of low-level exposure to antidepressant medication in breast milk are largely unknown. The risks of untreated maternal depression are well-known and significant. Some experts recommend that if medication treatment is indicated, clinical factors such as the patient’s prior response or nonresponse to an individual medication rather than data on blood levels should take precedence in the choice of first-line agent. 75 , 84 Decisions about initiating anti-depressant medication during breastfeeding and the choice of agent must be made on a case-by-case basis, and should involve a discussion of clinical factors, including severity of the depressive symptoms and prior response to medications and/or psychotherapy, known and unknown risks of the medication, the known risks of under- or untreated depression, and the patient’s preferences. 85 Regardless of which antidepressant medication a breastfeeding mother takes, the infant’s pediatrician should be made aware of the possible exposure, and the infant should be monitored for changes in feeding patterns, sleeping patterns, sedation, irritability and other signs of drug toxicity. As blood levels have not been correlated with adverse effects, routine laboratory testing of infant blood levels is not currently recommended.
Hormone therapy
There is a dramatic drop in maternal levels of estrogen and progesterone at the time of delivery, and this shift has been proposed as one trigger for the onset of PPD in some women. Effects of estrogen in the brain include the promotion of neuronal growth and survival, enhancement of neurotransmitter activity, mitigation of oxidative stress and modulation of the hypophyseal-pituitary axis. 86 A study designed to replicate the hormonal changes experienced around the time of birth found that women with a prior history of postpartum depression experienced mood symptoms when exposed to a drop in estradiol and progesterone, whereas women without a history of PPD did not. 87 This finding suggests vulnerability to hormone shifts in a subset of the population, and raises the possibility of hormonal intervention as a treatment or preventative intervention for PPD.
In a double-blind placebo-controlled study by Gregoire et al 61 women with postpartum depression were randomized to receive estrogen or placebo patches. 88 Breastfeeding women were excluded. Over the first month of treatment, women receiving estrogen showed greater and more rapid improvement in their symptoms as measured on the Edinburgh Postnatal Depression Scale and in clinical interviews. Women in the placebo group also improved, but maintained depression scores above the screening threshold. Neither group had complete remission of symptoms. The authors did not control for women receiving concomitant antidepressant medication, which was more common in the estrogen treatment group, making interpretation of the study results difficult. Additionally, women were included in the study up to 18 months postpartum, by which time the effects the postpartum drop in estrogen would likely have resolved. 86
Although an early naturalistic study suggested progesterone as a promising preventative therapy against recurrent postpartum depression, 89 , 90 the results of that study were contradicted by a subsequent double-blind, placebo-controlled trial that found an increase in depressive symptoms in women treated with norethisterone enanthate, a synthetic progestogen. 91 In this study, 180 women were randomized to receive one depot injection of norethisterone enanthate or one injection of saline placebo within 48 hours after delivery and were followed for three months. The investigators found that women who received the synthetic progestogen were more likely to develop depressive symptoms, more likely to have bleeding, and more likely to complain of exhaustion. A recent review of the above studies concluded that while the research on estrogen is promising but preliminary, there is no role for synthetic progestogens in the treatment of PPD, and that given the increased risk for depressive symptoms their use as contraception in this population is questionable. 92
Other studies without control groups support an effect of estrogen in the treatment of postpartum depression. A small prevention study found that when a slow taper of estrogen therapy was administered immediately after birth to 11 women with a history of postpartum psychosis or depression only one woman suffered a relapse episode. 93 Another small study treated 23 women with severe postpartum depression with sublingual 17-beta estradiol over 8 weeks, and found remission of symptoms in 19 of the women, which the authors correlated with increased serum estrogen levels in the subjects. 94 Both studies should be interpreted with caution, given the lack of a comparison group.
Although initial results for the use of estrogen in the treatment of postpartum depression are promising, additional methodologically sound studies are needed. 86 Furthermore, estrogen therapy should not be used in women with an increased risk of thromboembolism. Treatment with gonadal steroids can interfere with lactation, which should be discussed with women prior to initiating therapy. Long-term use of estrogen therapy can cause endometrial hyperplasia and slightly elevates the risk of endometrial cancer; although this risk can be mitigated by co-administration of progesterone, 86 the increase in depressive symptoms with progestogen seen in the Lawrie study complicates the implementation of this strategy.
Psychological and psychosocial treatments for postpartum depression
Many mothers with postpartum depression are hesitant to take antidepressants due to concerns about infant exposure to medication through breast milk or concerns about potential side effects, 95 and therefore often prefer psychological treatments. 49 , 50 , 96 Although relatively few studies have systematically investigated nonpharmacologic treatments for PPD, existing research supports the use of both psychological treatments (specifically interpersonal therapy, cognitive-behavioral therapy, and psychodynamic psychotherapy), as well as psychosocial interventions, such as nondirective counseling. A Cochrane meta-analysis of ten randomized controlled trials of psychosocial and psychological treatments for postpartum depression concluded that both psychosocial and psychological interventions are effective in decreasing depression and are viable treatment options for postpartum depression. 97
Interpersonal therapy (IPT)
Interpersonal therapy (IPT) is a time-limited treatment for major depression based on addressing the connection between interpersonal problems and mood, 98 which frames depression as a medical illness occurring in a social context. 99 In IPT, the patient and clinician select one of four interpersonal problem areas (role transition, role dispute, grief, or interpersonal deficits) as a treatment focus. Over the course of the therapy (typically 12–20 weeks), strategies are pursued to assist patients in modifying problematic approaches to relationships and in building better social supports. IPT has been adapted to address problem areas relevant to postpartum depression such as the relationship between mother and infant, mother and partner, and transition back to work. 100 The fact that IPT is both time-limited and problem-focused fits well with the demands of the postpartum mother.
Several studies, including one large-scale randomized controlled trial, have supported the effectiveness of IPT for treating postpartum depression. O’Hara and colleagues randomized 120 women with postpartum depression to receive 12 weekly 60-minute individual sessions of manualized IPT by a trained therapist versus control condition of a wait-list. 101 The women who received IPT had a significant decrease in their depressive symptomatology (measured by Hamilton Depression Rating Scale and Beck Depression Inventory) as compared to the wait-list group, as well as significant improvement in social adjustment scores. In another study by Clark et al 35 women with postpartum depression were assigned to individual IPT (12 sessions) versus mother–infant group therapy versus a wait-list condition. 102 Both IPT and mother–infant group therapy were associated with greater reduction in depressive symptoms as compared to the wait-list conditions. Both studies support the effectiveness of IPT as a treatment for PPD, though there is not enough data to suggest a specific benefit to IPT compared with other therapeutic modalities.
Two small open studies have evaluated group IPT for postpartum depression. Klier et al conducted a pilot study in which 17 depressed women in two different groups received 9 weeks of group IPT and 3 individual sessions. 103 Depression scores on two rating scales decreased significantly during the course of treatment, and gains were maintained at 6-month follow-up. However, there was a high attrition rate (6 out of 17), and the study was also limited by small sample size, lack of a control group, and lack of an independent rater. Similarly, Reay et al treated, in an open pilot trial, 18 women diagnosed with postpartum depression with 8 group IPT sessions, as well as two individual and one partner session. 104 Depressive symptoms decreased significantly, and these gains were maintained at three months. Compared to the previous study, the drop-out rate was low, and authors speculated that this might be due to childcare provided. However, two-thirds of the study participants were receiving antidepressant therapy concomitantly, limiting interpretation of the effect of this group intervention. While it is difficult to make conclusions about efficacy based on this pilot data, the study authors suggest that advantages to group over individual IPT for postpartum depression might include increased social support, normalization of problems, development of interpersonal skills in a group setting that can be translated to outside relationships, and minimization of stigma associated with PPD.
Cognitive behavioral therapy (CBT)
Cognitive behavioral therapy (CBT), a well-studied and effective treatment for major depression, 105 is based on the premise that both perceptions and behaviors are intimately linked to mood. CBT focuses on helping depressed patients to modify distorted patterns of negative thinking and to make behavioral changes that enhance coping and reduce distress. 106 There have been several trials assessing CBT alone or with other interventions for the treatment of PPD. In a randomized controlled psychotherapy-pharmacotherapy study, Appleby et al assigned 87 women with PPD to one of four conditions in a factorial design, varying based on treatment with either one or six sessions of CBT-based counseling, and treatment with fluoxetine or placebo. 52 All four treatment groups had significant improvement in depressive symptoms. Women who received six CBT sessions versus one had greater decrease in depressive symptoms. Six sessions of CBT plus placebo pill was as effective as treatment with fluoxetine plus one session of CBT, but there was no added benefit in the group receiving 6 counseling sessions in combination with fluoxetine. It should be noted that the counseling sessions were delivered by briefly trained nonspecialists, and six sessions of CBT may not be a sufficient representation of a standard course of treatment. In another combination medication-CBT study, Misri et al randomized 35 women with PPD and comorbid anxiety either to paroxetine monotherapy or paroxetine and 12 weekly manualized CBT sessions with a psychologist. 53 While both groups had significant decreases in depressive symptoms, there were no significant differences between the two groups in response rates, time to remission or dose of medication required, suggesting no measurable added benefit to the CBT treatment in combination with an SSRI over the 12 week study period, as consistent with Appleby’s findings. In a randomized controlled trial looking at the effectiveness of CBT versus a control condition, Prendergast and Austin assigned 37 women with PPD either to six weekly one-hour home-based CBT sessions delivered by early childhood nurses (ECNs) or to “ideal standard care”, which consisted of six weekly visits to ECNs in a clinic setting. 107 Both groups with PPD had significant mood improvement, though there was a nonsignificant trend towards CBT being more effective at six-month follow-up. Among study limitations, ECNs administering CBT were not experienced therapists, though they received CBT training prior to the study and supervision throughout. Additionally, the control group more closely resembled a supportive psychotherapy rather than no-treament. These studies support CBT interventions as helpful in the treatment of PPD, though they do not support an additional benefit to CBT in combination with pharmacotherapy and do not clarify a specific benefit of CBT for this population in comparison with other treatments. Two of these studies also suggest a role for the training of nonmental-health professionals in this modality.
Nondirective counseling
As compared with IPT or CBT, psychosocial interventions are unstructured and nonmanualized, and include nondirective counseling and peer support. Nondirective counseling (also known as “person-centered”) is based on the use of empathic and nonjudgmental listening and support. In the first notable study evaluating this intervention, Holden randomized 50 women with PPD to 8 weekly nondirective counseling sessions with a health visitor or routine primary care. 108 A health visitor in the UK is a public health nurse who conducts home visits with pregnant and postpartum women. This study found that the rate of recovery from PPD for counseling (69%) was significantly greater than that of the control group (38%). In a similar study conducted in Sweden, Wickberg and Hwang randomized 31 women with PPD to receive six nondirective counseling sessions by child health clinic nurses or routine primary care. 109 As in the Holden study, a significantly greater percentage of women in the treatment group (80%) had remission of depression than in the control group (25%). Study limitations include the removal of four study participants, two in each group, for more intensive mental health services due to illness severity.
Peer and partner support
Epidemiologic data as well as some prospective studies have consistently identified inadequate social support as a risk factor for developing postpartum depression, 110 – 112 thus raising the possibility of interventions aimed at increasing social supports as treatment options for perinatal depression. In a prospective cohort of pregnant Chinese women, Xie et al 112 found that low support in both the prenatal and postnatal time period was associated with increased risk for postpartum depression, with the highest risk for postpartum women who had low objective or practical support. The broad applicability of this study is limited by the demographics of its cohort (limited to married Chinese primiparous women without significant obstetric complications, rates of Caesarian delivery over 70%) and the use of a rating scale most validated in the Chinese population. However, the finding suggests that tangible social support, such as assistance with caring for the newborn, may be particularly important and helpful in the treatment of postpartum depressed mothers.
In a pilot study, CL Dennis 113 evaluated the effect of mother-to-mother support as delivered over the telephone on depressive symptomatology in a postpartum patient population identified as at high risk for PPD based on EPDS score >9. Standard postpartum care in addition to individualized telephone-based peer support resulted in a significant reduction in depressive symptoms at 8 weeks. More recently, in a larger randomized multisite trial, Dennis and colleagues demonstrated that high-risk postpartum women who received telephone-based peer support over 12 weeks were at lower risk for developing PPD (as defined by EPDS >12) compared to a control group receiving usual care. 114 Due in part to the telephone-based nature of the study, the investigators were unable to confirm the findings from rating scales with structured clinical interviews.
While poor partner support has been identified as an important risk factor for PPD, 9 few studies have investigated the role of the partner or other family support in recovery from PPD. In one survey study, shared activities, problem-focused information and assistance, and positive feedback from the partner decreased a mother’s likelihood of having depressive symptoms at 8 weeks postpartum. 115 A qualitative study examining factors identified by women who had recovered from PPD to be most important in their recovery found that “emotional support from partner”, “improved communication with partner”, “practical support from partner”, and “emotional support from friends” were rated as “essential” to recovery. 116 A small, nonblinded study by Misri et al examined the impact of partner support in the treatment of PPD. 117 In this study, 29 women with PPD were randomized to receive 7 sessions of psychoeducation with (support arm) or without (control arm) their partners. Relative to the control group, women in the partner group had significant reductions in depressive symptoms, while the partners in this group may also have had protective benefit on measures of general health. These studies do not provide enough data to recommend a specific partner-based intervention, but they do suggest that including the partner in the treatment of PPD may be of benefit for some women.
Comparisons of psychological and psychosocial treatments
Cooper et al designed a large study to assess the effects of different psychological interventions on PPD. 118 A community sample of 193 women with PPD were randomized to receive from weeks 8–18 postpartum routine primary care versus one of three treatment conditions: CBT, psychodynamic psychotherapy, or nondirective counseling. All three treatments decreased depressive symptoms significantly as measured by EPDS at 4.5 months, in comparison to no treatment. Rates of remission from depression, as defined by DSM-III, were higher for those receiving psychodynamic therapy (71%) than CBT (57%) or nondirective counseling (54%). However, there were no differences among any of the groups at the 9 month assessment. Milgrom et al also undertook a study to compare different psychological interventions for PPD. 119 A community of 192 women with PPD were randomized to routine primary care or 12 weeks of group-based CBT, or group-based or individual counseling utilizing supportive therapy techniques delivered by trained therapists. All three psychological interventions were superior to routine care in reducing symptoms of PPD. While there were no significant differences between counseling and CBT, individual counseling was slightly more effective than group counseling. Finally, Morrell et al in a large, cluster randomized trial, looked at an intervention that trained health visitors to identify depressive symptoms in postnatal women and to deliver either a cognitive behavioral or nondirective “person-centered” approach involving up to eight sessions of individual counseling. 120 They compared this with usual care delivered by health visitors who did not receive this training, in conjunction with general practitioners. In this study, women who had an EPDS score ≥12 at 6 weeks postpartum were followed for 18 months. At 6 months, significantly more women in the control condition remained with elevated EPDS scores compared to both intervention groups, and the differences persisted at 12 months. There were no differences between the two counseling approaches. While the specific effective component of the intervention was unclear, this study does provide evidence that training in psychologically-informed approaches for non mental-health providers can significantly enhance the care of depressed postnatal women.
A recent meta-analysis compared psychological and psychosocial interventions for PPD, including CBT, IPT, and nondirective counseling, as well as peer support. 121 This study did not find any difference in effect size for any of these treatments, and concluded that different types of psychological interventions seem equally effective for treatment of PPD.
In summary, both psychological and psychosocial interventions for PPD have shown benefit over no treatment or “usual care” in multiple studies. Further studies are needed to discriminate between the effectiveness of various psychological and psychosocial treatments for PPD and between group-based and individual modalities.
Other nonpharmacologic treatments for postpartum depression
Many women suffering from PPD and their healthcare providers may seek alternatives or adjuncts to standard psychological or pharmacologic treatments because of their concern about the effects of pharmacological treatment on breastfeeding, 122 access to care, issues of stigma in the treatment of mental illness, limited effectiveness, or personal beliefs. In the following we have provided an overview of a variety of evidence-based nonpharmacologic treatments for postpartum depression.
Electroconvulsive therapy
As with treatment-refractory major depression in the general population, electroconvulsive therapy (ECT) is an option for depressed postpartum women who do not respond to antidepressant medication or who have severe or psychotic symptoms. Data specific to this population are very limited. One small study of 5 women receiving ECT for refractory postpartum depression reported a 100% remission rate. 123 Apart from concerns regarding anesthesia and breast feeding, the use of ECT for postpartum depression does not differ from its use in major depression. 124 Anesthetic agents used in ECT are typically rapidly metabolized, and risk of transmission in breast milk can be minimized by timing breast feeding accordingly.
Bright light therapy
While bright light therapy was initially introduced as a treatment for seasonal affective disorder, research has supported its effectiveness as a treatment for nonseasonal depression. 125 Light therapy presents an attractive option for the treatment of perinatal depression, as there are no known risks to the fetus or nursing infant. However, despite some encouraging preliminary data in antenatal depression, 126 there is currently insufficient data on its effectiveness in the postpartum population. In one study, 127 15 outpatient women with PPD were randomly assigned to receive bright light (10,000 lux, n = 10) or dim red light (600 lux, n = 5) daily for six weeks. This study was unable to elicit a specific treatment effect of the light therapy due to the small sample size, though both groups showed significant improvement over time on all measures of depression. Further studies are required to clarify the effectiveness of light therapy in the treatment of postpartum depression.
Omega-3 fatty acids
Omega-3 fatty acids have received specific attention in the treatment of perinatal depression, because of the known health benefits of these compounds for pregnant and postpartum women as well as some data showing positive effects on mood in the general population. 128 Omega-3 fatty acids such as the eicosapentaenoic acid (EPA) and docosa-hexaenoic acid (DHA) found in fish oils, are the key building blocks for the development of a baby’s central nervous system while in utero, 129 and depletion of maternal omega-3 fatty acids occurs during pregnancy to facilitate this process. 130 One often-cited cross-national study 131 evaluating major depression in the general population demonstrated that per capita fish consumption was inversely related to the risk of developing major depression. Further epidemiologic data support an association between low omega-3 intake from seafood and increased risk of high levels of depressive symptoms during pregnancy. 132
Despite these epidemiologic associations, studies examining the use of omega-3 fatty acids for treatment of perinatal depression have had mixed results. Freeman et al conducted two pilot studies of omega-3 fatty acids as an intervention for perinatal depression; one was an open-label flexible-dose trial of a combination of EPA and DHA for the treatment of MDD during pregnancy, 133 and the second trial assessed the efficacy of omega-3 fatty acids for postpartum depression in an 8-week randomized dose-ranging study. 134 The outcome of the first trial showed a 40.9% mean decrease in depressive symptoms on the Edinburgh Postnatal Depression Scale. The second study, a randomized dose-ranging trial for postpartum depression found no significant difference between control and study group. Both studies were limited by their small sample sizes (n = 15 and 16, respectively) and their lack of a placebo group. A subsequent randomized placebo-controlled study investigating the combination of omega-3 fatty acids and supportive psychotherapy for the treatment of perinatal depression 135 again demonstrated no significant difference between the omega-3 fatty acids and placebo, though participants in both groups experienced significant decreases in their depression rating scales. The benefits of supportive psychotherapy received by both groups may have limited the ability to detect a specific effect of omega-3 fatty acids. A subsequent small, randomized, double blind, placebo-controlled trial investigating omega-3 fatty acids at a dose of 3.4 g per day as monotherapy for major depression during pregnancy 136 demonstrated a benefit from this intervention. Although there was relatively high attrition in both groups, subjects receiving omega-3 fatty acids had significantly lower scores on depression rating scales as compared to the placebo group at the study end point.
In sum, omega-3 fatty acids may have therapeutic benefits for perinatal depression, but thus far most studies investigating this effect have been limited by small sample sizes. Some of these studies 135 did establish that dietary intake of omega-3 fatty acids among participants was low prior to study involvement. Omega-3 fatty acids have clear health advantages for both the mother and for the developing fetus or nursing infant. Of note, omega-3 fatty acids can increase bleeding times at high doses, but according to a recent study, 137 omega-3s at doses of 3–4 g/day produced no clinically significant increase in bleeding times or in bleeding events in patients with cardiovascular disease already treated with anti-platelet agents.
Acupuncture and massage
Acupuncture is the ancient Chinese tradition of the inserting and manipulating needles into various points on the body to treat pathologic processes and relieve pain. It has been investigated for the treatment of depression in the general population with mixed results, 138 and has been increasingly investigated as adjunctive treatment in pregnancy for nausea, pain, breech presentation and induction of labor. 139 There is no data about the use of acupuncture in postnatal depression, but one small pilot study by Manber et al compared the effectiveness of targeted acupuncture vs controls of a nontargeted acupuncture and massage in the treatment of pregnant depressed women. 140 8 weeks of an active acupuncture intervention targeted specifically for depression (treatments were standardized but individually tailored) significantly outperformed a massage intervention in terms of reduction of depressive symptom rating scales in depressed pregnant women. While there was no significant difference in symptom reduction between the targeted and control acupuncture treatments in this study, a more recently published larger randomized trial of acupuncture in pregnant women showed significant reduction in depressive symptoms in active treatment versus both control conditions. 141 The authors caution that the study was not designed to assess the effectiveness of massage as a treatment for perinatal depression. It is not clear what the effects of antenatal or postnatal acupuncture are on postnatal depression. It should be noted that as acupuncture may have effects on induction of labor and lactation, 138 , 142 women who wish to try acupuncture as a treatment or adjunctive therapy for perinatal depression should be sure the practitioner is experienced in these issues.
Massage as treatment for perinatal depression has also been examined independently, and modalities include therapeutic massage, partner-delivered massage, and instruction in infant-massage in the postpartum period. Field et al looked at the effect of 10 sessions of massage versus 10 sessions of relaxation techniques in 32 adolescent inpatients with postnatal depression, and found a significant improvement in depression ratings in the massage group after session 10 but not the relaxation group. 143 There was no longer-term follow up, so the clinical implications of this study are limited. Another study looked at the effects of infant massage, and compared the effects of 15 minutes of rocking versus 15 minutes of massage on 40 full-term infants between the ages of 1 and 3 months born to depressed mothers. 144 They found multiple benefits for the infants in the massage group, including improvements in sleep patterns, interactions, crying, weight gain, and lower cortisol levels, though there was no measure of effects on maternal depression. Onozawa et al 145 compared outcomes in mother–infant pairs who received 5 weekly sessions of infant massage classes plus a support group with mothers who were in a support group alone. Depression scores in both groups decreased without significant difference, but only the infant massage group showed statistically significant improvement in global ratings of mother–infant interactions. However, there was high drop-out in this study, and significant improvement in the massage group occurred prior to the first class, suggesting nonspecific or anticipatory benefit. A subsequent trial with a similar design 146 failed to demonstrate these same advantages in mother–infant interactions after six sessions of infant massage compared to support groups alone, and depression scores in both groups again improved similarly. A more recent study investigated maternal massage therapy administered by the woman’s partner for 12 weeks 147 in depressed pregnant women and found benefit in the massage group on indices of depression during late pregnancy and immediately postpartum, as well as lower cortisol levels in mothers and neonates. However, the control condition was unspecified standard care, and as there was no longer term follow-up the impact of the intervention on PPD is unclear. In summary, massage in its various forms described above has few risks, and may have benefits for women and their infants, but its effectiveness as a treatment for PPD remains in question.
Several studies have investigated the role that exercise can play in alleviating postpartum depressive symptoms. 148 A study by Da Costa et al looked at 88 women with PPD who were randomized to a 12-week, home-based exercise program or usual care. 149 There was a reduction in depression rating scales in the intervention group as compared to the usual care group post-treatment, though not at the 3-month follow-up. However, Ko et al 150 investigated a low-intensity exercise program that was specifically designed and administered to women with postpartum fatigue and depression. There was no significant change in depression between the treatment group and the control group. Despite the limited evidence of efficacy for treatment of PPD, 151 the UK National Institute for Health and Clinical Excellence (NICE) 152 has recommended in their antenatal and postnatal mental health guidelines that health professionals should consider exercise as a management strategy in women experiencing mild-to-moderate depression. A review of the effects of exercise on PPD defined “feasible and effective” exercise as: moderate-intensity activities for at least 30 minutes per day, five days of the week, including walking in the form of “pram pushing”. 153
Postpartum depression is a major international public health problem that affects at least 1 in 8 mothers and their children in the year after childbirth worldwide. PPD may be more common and may be associated with more morbidity for both mothers and children in resource-poor countries. PPD has been associated with significant negative effects not only on depressed women themselves, but on the physical, cognitive and emotional development of their children. Early detection and intervention are important in mitigating these risks. There are validated and easily administered screening tools for PPD available in many languages, such as the Edinburgh Postnatal Depression Scale; most experts recommend screening women for PPD 4–6 weeks after delivery.
Psychopharmacologic treatment of PPD is complicated by both known and unknown risks of medication in breast milk. There have been few medication trials specifically evaluating the effectiveness of antidepressant medication or ECT for postpartum depression, but the available evidence suggests that medications typically used to treat major depression in the general population are equally effective in postpartum depression. All medications pass into breast milk, though the extent of passage varies considerably between drugs, and sertraline, paroxetine and nortriptyline currently appear to have the best safety profiles in breastfeeding. There have been case reports of adverse effects in nursing infants of antidepressant medication in breast milk, but the advantages of breastfeeding to the mother and infant may outweigh the risks of exposure. Exposed infants should be monitored for any acute behavioral changes. However, the long-term risks of medication exposure to the infant remain unknown. Most experts recommend that the choice of medication in the postpartum should be based first on known efficacy for an individual woman, and that known milk-plasma ratios should be a secondary consideration unless a patient is treatment-naïve. Some studies suggest that estrogen may be an effective agent for treatment, prevention or augmentation in depressed postpartum women; however data remains limited and there are significant health considerations with hormonal intervention.
Psychological treatments for PPD are often the treatment of choice for women, as they are effective for the treatment of depressive symptoms and do not involve the risks of exposure to medications. Research supports both psychotherapy and other psychosocial interventions as effective in mitigating symptoms of PPD. Interpersonal psychotherapy, cognitive behavioral therapy, psychodynamic psychotherapy and other supportive interventions such as telephone-based peer support, counseling by a health visitor, and partner support have also shown benefit over wait-list or usual care controls.
Other nonpharmacologic interventions that have been studied in the treatment of PPD include bright light therapy, acupuncture, massage, omega-3 fatty acid supplementation, and exercise. Data on the effectiveness of these modalities in decreasing maternal depressive symptoms is limited, but these interventions have minimal risks and may have health benefits for both mother and infant.
The authors report no conflicts of interest in this work.

IMAGES
COMMENTS
Postpartum depression is widely recognized as a significant health threat to the mother and the rest of the family, and thus to society, but the biggest threat is to the lifetime health prospects of the newborn infant. Given the health significance of postpartum depression, recent research about the risk factors for this condition, and ...
Postpartum depression (PPD) is a significant mental health constraint in females, which has an effect on nearly 13-19% of the females who newly attained motherhood . PPD is identified by a continuous feeling of a low state of mind in new mothers, followed by sad feelings, less worthy, and despondence. It differs from baby blues, a short-lived ...
Activity During Pregnancy and Postpartum Depression. Studies have shown that women's mood and cardiorespiratory fitness improve when they engage in moderate-intensity physical activity in the weeks and months after giving birth to a child. Complementary Therapy for Postpartum Depression in Primary Care. Thus, the woman faced frustration and ...
Excessive irritability, anger, or agitation; mood swings. Sadness, crying uncontrollably for very long periods of time. Fear of not being a good mother. Fear of being left alone with the baby. Misery. Inability to sleep, sleeping too much, difficulty falling or staying asleep. Disinterest in the baby, family, and friends.
The typical signs of postpartum depression include the presence of sleep disorder, fatigue, crying, anxiety, changes in appetite, and feelings of inadequacy (Tharpe, Farley, & Jordan, 2017). The patient has these symptoms, which allowed for establishing the diagnosis. Drug therapy included the prescription of tricyclic antidepressants, as they ...
Postpartum Depression has many underlying causes and cannot be narrowed down to one single factor. However, mental and physical changes after birth can definitely make an impact on the manifestation of PPD. Every woman experiences changes in their body after giving birth. However, the body changes come with hormone changes, and the hormones ...
Studies show that postpartum depression is high among women who are physically and psychologically traumatized. For instance, women restricted to refugee camps and reservations can easily acquire PPD. Women living in such confined areas results in decreased economic opportunities and social support. Gaining access to education or services, such ...
Go to: Postpartum depression (PPD) is an irritable, severely depressed mood that occurs within 4 weeks of giving birth and possibly as late as 30 weeks postpartum. Manifestations include crying spells, insomnia, depressed mood, fatigue, anxiety, and poor concentration. Patients may experience mild, moderate, or severe symptoms.
Postpartum depression. Your body and mind go through many changes during and after pregnancy. If you feel sad, anxious, or overwhelmed or feel like you don't love or care for your baby and these feelings last longer than 2 weeks during or after pregnancy, you may have postpartum depression. Treatment for depression, such as therapy or ...
Unlike the baby blues, a mother with postpartum depression feels worse over time and changes in her behavior does not go away on their own even with the help of their loved ones. Postpartum major mood disorder depression, or postpartum depression (PPD), affects from 10% to 16% of postpartal women. This statistics simply implies the importance ...
Postpartum depression is a debilitating mental disorder with a high prevalence. The aim of this study was review of the related studies. In this narrative review, we report studies that investigated risk factors of postpartum depression by searching the database, Scopus, PubMed, ScienceDirect, Uptodate, Proquest in the period 2000-2015 published articles about the factors associated with ...
Essay grade: Excellent. 3 pages / 1375 words. Imagine being locked in a room, with no outside interaction, except for the rare conversations with a housemaid or husband. Add in a bout of postpartum depression and an overbearing husband to have the story of Jane, a woman in nineteenth-century America.
Studies show that new fathers can experience postpartum depression, too. They may feel sad, tired, overwhelmed, anxious, or have changes in their usual eating and sleeping patterns. These are the same symptoms that mothers with postpartum depression experience. Fathers who are young, have a history of depression, experience relationship ...
For these reasons, hormone therapy may play a role in managing postpartum depression. Side effects of hormone therapy with estrogen may include: weight changes. nausea and vomiting. abdominal ...
Postpartum depression is a common and complex phenomenon that can cause relevant negative outcomes for children, women and families. Existing literature highlights a wide range of risk factors. The main focus of this paper is to jointly investigate different types of risk factors (socio-demographic, psychopathological, relational, and related ...
Results: A total of 122 studies (out of 3712 references retrieved from bibliographic databases) were included in this systematic review. The results of the studies were synthetized into three categories: (a) the maternal consequences of postpartum depression, including physical health, psychological health, relationship, and risky behaviors; (b) the infant consequences of postpartum depression ...
And too often, another consequence of labeling postpartum upset and suffering as mental illness is that the woman is put on psychiatric drugs that, as always with such drugs, can sometimes help ...
This essay will examine several recent research articles and what they offer in terms of best practice approaches for treating women at risk for postpartum depression. Prospective mothers often ask their psychiatrist if there is a risk that they might abuse their child (reviewed by Choi et al., 2010).
Postpartum depression (PPD) is a mental health disorder that affects 10%-15% women globally. Longitudinal and meta-analyses have consistently demonstrated the negative impacts of PPD on both the affected mothers and subsequent infant development. ... This is the first study to outline the roles of social support (psychoeducation, nurses ...
Postpartum mood disorders, including postpartum depression (PPD), anxiety disorders, and even rare but severe cases of postpartum psychosis, can cast a shadow over what is meant to be a joyous time. The significance of this topic lies in the potential long-term consequences of untreated postpartum mood disorders, affecting not only the mother ...
Post-Partum Issues -- Effects on Child Development A peer-reviewed article in the journal Child Psychiatry and Human Development points out in the Abstract that there is a strong association between "maternal psychological distress and infant outcomes" (Kingston, et al., 2012, p. 683). In fact the article asserts that indeed, parental distress -- in particular postpartum depression and related ...
Postpartum depression (PPD) is a mood disorder that affects individuals within 1 year after childbirth. According to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), postpartum depression is now included in the term perinatal depression.[1] A major depressive episode that begins during pregnancy or within 4 weeks after delivery is classified as peripartum depression.
Sub-analyses of this study revealed an improvement in maternal role function 56 and sexual function 57 that was equivalent in both groups. Several open studies have found sertraline, 58 venlafaxine, 59 nefazodone, 60 fluvoxamine, 61 and bupropion 62 to be effective in the treatment of postpartum depression. These studies have been small, with 4 ...